Impact of COVID-19 in Africa: A scenario analysis to 2030 (July 2020)
Summary
- This study was completed in July 2020 - one of the first on the long-term impact of COVID-19 on Africa. We found that COVID-19 is set to undo several years of development progress in Africa. Jump to Comparative outcomes: V, U, L scenarios
- Compared to the pre-COVID-19 forecast, Africa’s economy will be between US$335 billion and US$617 billion smaller in 2030. Jump to Comparative outcomes: V, U, L scenarios
- In a best-case scenario, GDP per capita will recover to 2019 levels in 2024. In the worst case, Africa will only return to 2019 levels in 2030. Jump to Three COVID-19 scenarios
- Efforts to roll out additional social grants in several African countries to mitigate the impact of the pandemic will marginally reduce extreme poverty and income inequality in the short term. Jump to Comparative outcomes: V, U, L scenarios
- Relative to the pre-COVID-19 forecast, 14 million additional Africans will be extremely poor in 2020. In 2030, an additional 38 to 70 million more people would be classified as extremely poor. This translates to poverty rates of between 35% and 37% of Africa’s total population. Jump to Comparative outcomes: V, U, L scenarios
- COVID-19 is set to further constrain Africa’s progress towards attaining the 2030 Sustainable Development Goals. Jump to Comparative outcomes: V, U, L scenarios
- The pandemic is expected to significantly reduce government revenue and health expenditure and undermine debt sustainability in several African countries. In the worst case, more people will have died from the impact of reduced health expenditure and hunger by 2030 than from COVID-19. Jump to Three COVID-19 scenarios
Recommendations Jump to Policy Reponses and recommendations
African countries should
- continue to act proactively in responding and adapting to new information and strategies to tackle COVID-19.
- efficiently manage existing resources to contain COVID-19 and other structural challenges.
- Increase transparency and practise more responsible borrowing.
- grow their tax base and improve tax collection systems.
- take advantage of the opportunity to accelerate digitisation of their economies to improve resilience, productivity and ability to reap the benefits of the 4th industrial revolution.
- re-engineer sectors like health and WaSH to better cater to the needs of people in rural and urban areas.
The African Union should:
- call for better procurement systems and action plans for African countries to acquire health equipment amidst high global demand and competition.
- advocate for debt moratoriums and relief for African countries.
- spearhead the implementation of the African Continental Free Trade Agreement as a means to unlock economic diversification and more rapid growth.
- promote an African response framework and medical research partnerships for COVID-19, and lead on disease and public health surveillance on the continent.
International development partners and civil society should:
- provide debt relief and insist on full transparency on all loans.
- support the provision of healthcare and basic infrastructure.
- assist Africa’s response to COVID-19 through continued financing and capacity building in key sectors like health.
- draw attention to human rights issues to keep governments accountable in their response to COVID-19.
All charts for Impact of COVID-19 in Africa: A scenario analysis to 2030 (July 2020)
- Chart 3: Framing of scenarios
- Chart 5: Growth rates: Africa under different scenarios vs rest of the world
- Chart 6: GDP per capita under different scenarios
- Chart 7: Decline in GDP per capita: 2020 compared to 2019
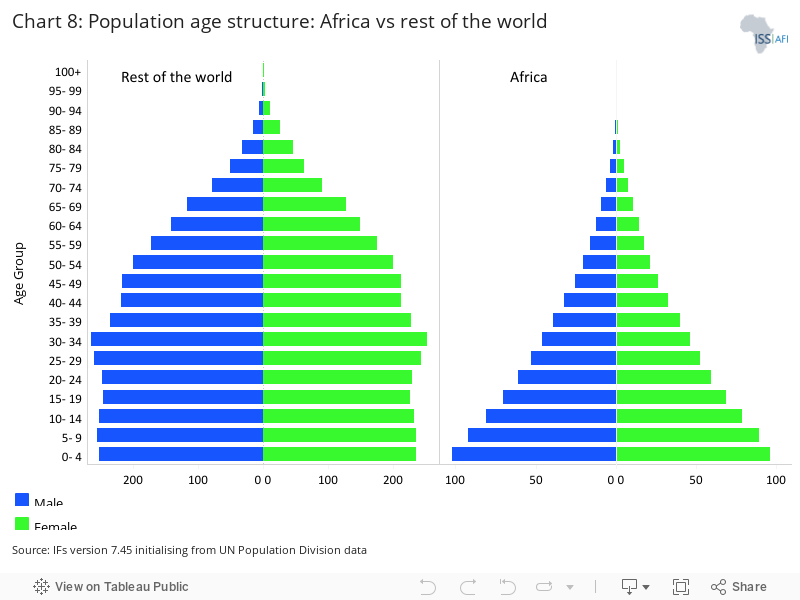
- Chart 8: Population age structure: Africa vs rest of the world
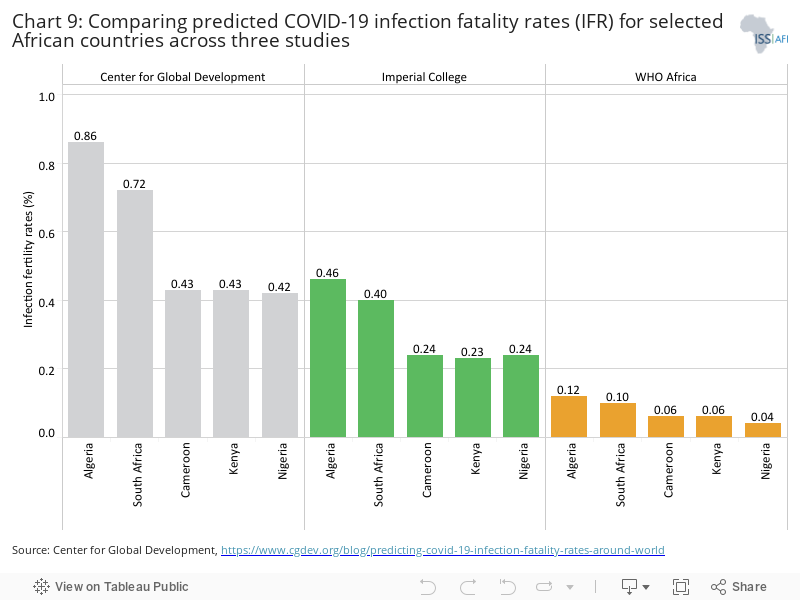
- Chart 9: Comparing predicted COVID-19 infection fatality rates (IFR) for selected African countries across three studies
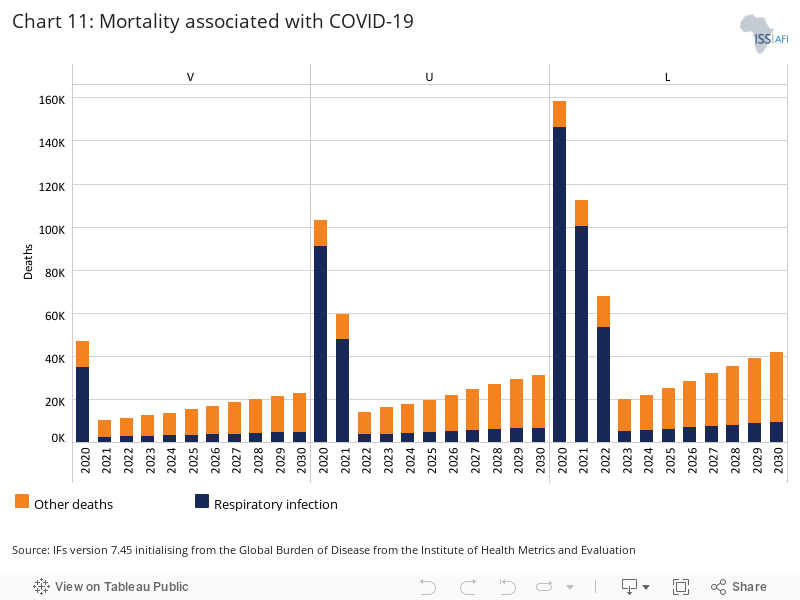
- Chart 11: Mortality associated with COVID-19
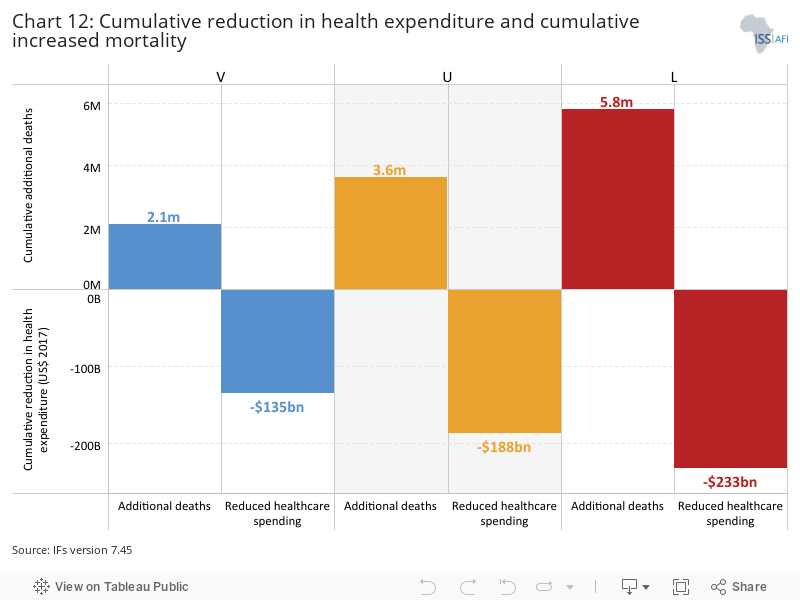
- Chart 12: Cumulative reduction in health expenditure and cumulative increased mortality
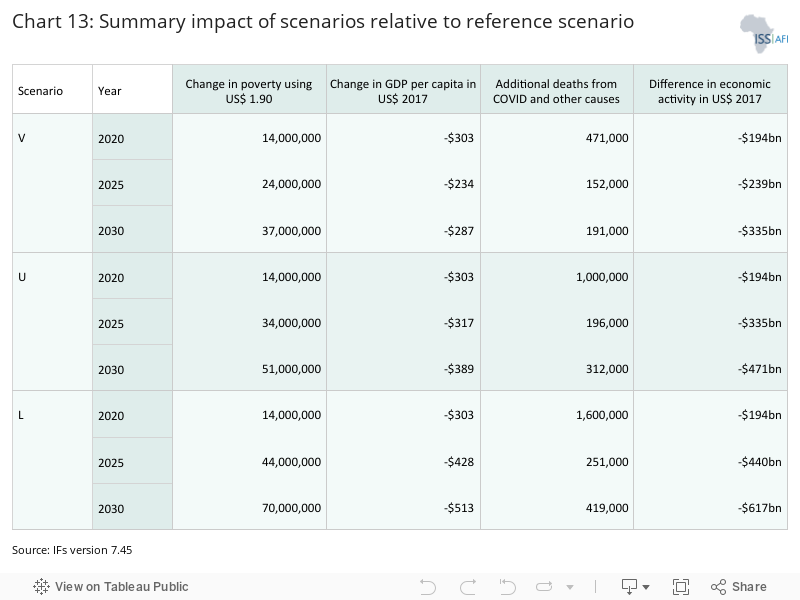
- Chart 13: Summary impact of scenarios relative to reference scenario
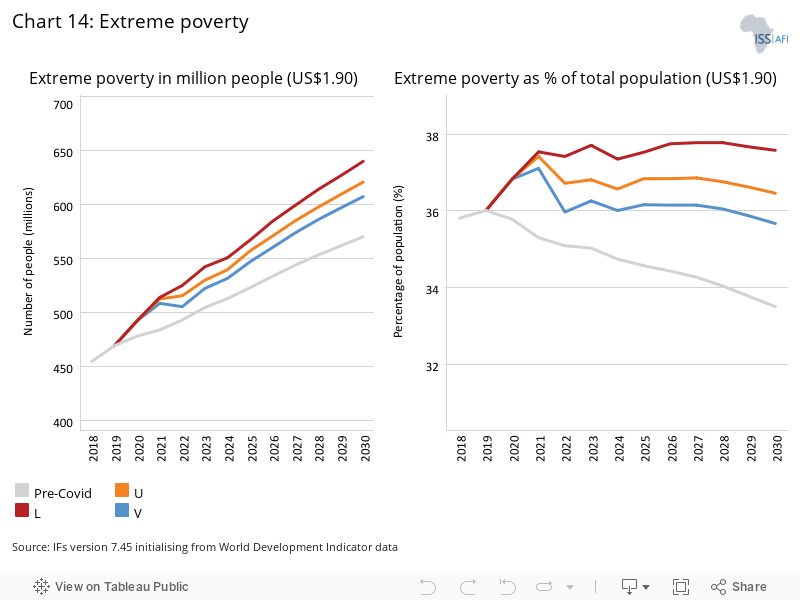
- Chart 14: Extreme poverty
This report presents three scenarios on the potential impact of COVID-19 in Africa and compares that to a pre-COVID-19 baseline, using the International Futures (IFs) forecasting platform. The likely impacts are then examined on economic growth, per capita income, poverty and the attainment of selected Sustainable Development Goals (SDG) targets with a forecast horizon to 2030. [1For a useful mapping of the Sustainable Development Goals and targets to the African Union’s Agenda 2063, see: United Nations Economic Commission for Africa (UNECA), Integrating Agenda 2063 and 2030 Agenda for Sustainable Development into national development plans, 2017]
The report concludes with four main policy recommendations aimed at reducing vulnerability and strengthening Africa’s resilience. These recommendations aim to make a robust contribution to the debate about policy options for Africa facing the international community, African governments and in-country stakeholders.
In addition to the scenarios presented in this report, a parallel qualitative approach involved a series of three dialogues that provided a platform for deliberation between economists, political analysts, public health experts and other development practitioners from Africa as well as global experts on Africa. The focus of the dialogues was on 15 African countries considered to be broadly representative of Africa’s developmental, regional and cultural diversity. [2Algeria, Tunisia, Mali, Sierra Leone, Nigeria, Cameroon, Chad, Sudan, Ethiopia, Kenya, the Democratic Republic of the Congo (DR Congo), Angola, Malawi, South Africa and Mauritius.]
Participants had an opportunity to share perspectives with counterparts, test their assumptions about alternative future scenarios for the pandemic in Africa, and comment on various iterations of the scenarios presented in this report. Perspectives from the dialogues are woven into this report and are more fully reflected in a report to be issued by the Gordon Institute of Business Science titled Navigating the Post-COVID Business Environment in Africa: An Alternative Scenarios Approach.
For validation and feedback, the successive versions of the macro scenarios in this report were presented to the roughly 100 participants of the dialogue sessions, as well as to a project reference group comprising representatives of development agencies and experts. In addition, the scenarios were circulated for comment by means of a questionnaire with a request for detailed feedback. A separate presentation was made to macro-economic experts at the United Nations Economic Commission for Africa (UNECA) as well as a small group of public health experts. As such, this report synthesises the combined perspectives of a wide-ranging and inter-disciplinary community of experts.
The World Health Organization (WHO) acknowledged COVID-19 as a Public Health Emergency of International Concern on 30 January 2020. Africa experienced its first case on 14 February, in Egypt, and COVID-19 was declared a global pandemic on 12 March. Two months later the disease had spread to every country in Africa, mostly entering capital cities through international flights from Europe and spreading from there through community transmission.
To date, mortality rates in Africa are significantly lower than elsewhere, generally attributed to Africa’s more youthful population. Community transmission is however now accelerating in most countries. The pandemic is spreading particularly rapidly in South Africa, which has the largest number of cases, although most deaths in Africa attributable to COVID-19 have occurred in Egypt. [3Africa Centres for Disease Control and Prevention (CDC), Coronavirus Disease 2019 (COVID-19)] While the veracity of testing and case data in Africa is questionable, the impact of the pandemic is uneven. Other highly affected countries include Algeria, Morocco, Nigeria and Ghana.
While it took 98 days for Africa to reach the first 100 000 cases, it took only 18 days for that number to double and the rate continues to accelerate. [4WHO, Rolling updates on coronavirus disease (COVID-19)] For much of Africa, it seems likely that the larger infection and mortality impact of COVID-19 is still to come.
Early efforts to contain the spread through travel restrictions, lockdowns and market closures have played an important role in constraining rates of infection in many countries but have taken a heavy social and economic toll. Some countries, such as Tanzania, have taken limited measures against the virus and in April 2020 stopped updating public information relating to the pandemic.
The impact of the pandemic has been described by the UN as ‘the greatest test that we have faced since the formation of the United Nations’ [5 United Nations, UN launches COVID-19 plan that could ‘defeat the virus and build a better world’, UN News, 31 March 2020], and by the International Monetary Fund (IMF) as ‘the worst economic fallout since the Great Depression’. [6International Monetary Fund (IMF), Confronting the Crisis: Priorities for the Global Economy, speech by Kristalina Georgieva, IMF managing director, Washington, DC, 2020]
The UN Development Programme expects the decline in the Human Development Index in 2020 to erase all progress made in human development worldwide over the past six years. [7United Nations Development Programme (UNDP), Human Development Reports, COVID-19 and Human Development: Assessing the Crisis, Envisioning the Recovery, 2020, p.6] Globally, more than US$8 trillion has been committed to fighting the associated health, economic and other effects — an amount several times larger than the combined GDP of Africa.
|
Chart 1: The project was implemented by the African Futures & Innovation programme at the Institute for Security Studies (ISS), the Centre for Leadership and Dialogue at the Gordon Institute for Business Science (GIBS) in Johannesburg and the Frederick S. Pardee Center for International Futures at the University of Denver, United States. Funding was provided by Humanity United and the Hanns Seidel Foundation. |
At first blush Africa appeared to many to be particularly susceptible to COVID-19, due to the continent’s crowded informal urban settlements and the challenges these pose to the implementation of measures such as social distancing.
In addition, many African countries have relatively low levels of access to safe water, generally considered the first line of defence against COVID-19. They also have high levels of undernourishment, poorly funded health systems and underlying health conditions such as tuberculosis and HIV/Aids. The average percentage of the population in Africa with improved water access was 78% in 2019, compared to the average for the rest of the world of 96%. In Africa, only Mauritius, Algeria, Egypt, Tunisia, Cape Verde, Botswana, Seychelles, and São Tomé and Príncipe are above the average for the rest of the world.
Furthermore, countries in sub-Saharan Africa generally spend significantly less on health as a percentage of GDP compared to all other regions globally, except South Asia. [8Average health expenditure in sub-Saharan Africa is roughly 2.6% of GDP. It is three times that in North America and in Europe.] Many African countries adopted public health and mitigation measures taken by states that were more advanced in their response to the pandemic, such as China, and generally reacted rapidly despite limited resources and capacity. Countries closed their borders and some embarked on a comprehensive lockdown strategy, accompanied by contact tracing to map transmission clusters and isolate people suspected of being infected.
A number of countries, such as Uganda and South Africa, rapidly established expert panels to guide their pandemic response. Others, such as Ghana, decided against a full lockdown, opting instead for a partial one, backed by vigorous contact tracing and monitoring. Rwanda disinfected and decongested its food markets and provided sanitary facilities along key rural-urban public transport corridors, while Senegal established mobile teams that targeted their response to where the disease was reported. [9Africa Center for Strategic Studies, African Adaptations to the COVID-19 Response, 15 April]
The intention was to flatten the rate at which COVID-19 infections increase, buy time for public officials to improve the capacity of health systems, and improve their readiness to deal with the anticipated full impact of the pandemic. The continent was able to benefit from the experiences gained from previous diseases such as Chikungunya. Some 41 African countries have experienced at least one epidemic, such as the Ebola epidemics of 2014-16 in West Africa and 2018-2020 in the Democratic Republic of the Congo (DR Congo), and recurrent Lassa fever epidemics in Nigeria. [10A Otu, B Ebenso, R Labonte and S Yaya, Tackling COVID-19: Can the African continent play the long game?, Journal of Global Health, 10:1, 2020, 10339. Note: Chikungunya is a viral disease transmitted to humans by infected mosquitoes. It has been identified in over 60 countries globally, including most prominently in the DR Congo and Gabon. Lassa fever is an acute viral haemorrhagic illness caused by the Lassa virus. It is endemic in Benin, Ghana, Guinea, Liberia, Mali, Sierra Leone, Togo and Nigeria.]
While some countries such as New Zealand have been able to reduce infection rates through a comprehensive set of interventions, some of these measures are difficult to implement effectively in much of Africa. This is due to low state capacity, widespread poverty, high levels of informality and the absence of adequate social safety nets on the continent.
Flattening the COVID-19 infection curve therefore might avert the collapse of a national health system but potentially have far-reaching impacts on the economy and livelihoods. In addition, with fewer hospital beds, physicians and intensive care facilities per million people than other regions, most African health systems will be unable to cope once infection rates accelerate, as is expected to happen in the latter half of 2020.
New medicines will help in responding to COVID-19. In mid-June the use of the well-known and relatively inexpensive steroid dexamethasone was hailed as the first major breakthrough in the treatment of patients who are severely ill with the coronavirus.
Dexamethasone is claimed to reduce deaths by one-third in severely affected patients in need of ventilation and by one-fifth in patients receiving oxygen only, but there was no benefit among patients who do not require respiratory support. [11World Health Organization (WHO), WHO welcomes preliminary results about dexamethasone use in treating critically ill COVID-19 patients, 16 June 2020] Other medical treatments will inevitably follow with important impacts on the mortality forecasts referred to in this and other reports. Without effective medicine or a vaccine that can be manufactured and rolled out on a massive scale, COVID-19 will affect Africa for some time to come.
Countries such as Sweden, with much more health capacity than African states, experimented with an alternative approach. It opted not to institute a lockdown and allow for the development of herd immunity instead but is now moderating its policies. [12R Haussman, Managing COVID-19 in the Americas, Africa and the Middle East, 29 May 2020] Herd immunity would probably require that up to 80% of the total population becomes infected. There would be large health, economic, social and political uncertainties on the path to that level of immunity — bearing in mind that at current methods and levels of testing most countries are below infection rates of 10%
The potential health, economic, social and political impact of infection rates of 30%, 50% or 70% of a total population are currently unknown and a lot depends on the symptoms and severity with which people are affected. Our current limited insight and data about why the pandemic is spreading so unevenly in Africa may result in an outcome where COVID-19 settles into an endemic equilibrium, as is the case with seasonal flu.
Africa and the rest of the global community may learn to live with COVID-19. And, as we explore below, the current low transmission, fatality and infection rates in Africa indicate large uncertainties as to how the pandemic will ultimately affect the continent.
The growth forecast released by the IMF in October 2019 serves as the basis for a pre-COVID-19 Reference scenario against which alternative pathways can be measured. The IMF forecast an average of 2.6% growth for Africa in 2020. Initialising from this rate, the forecast from IFs was for Africa to experience an average of 3.8% growth from 2020 to 2030.
|
Chart 2: Project notes
|
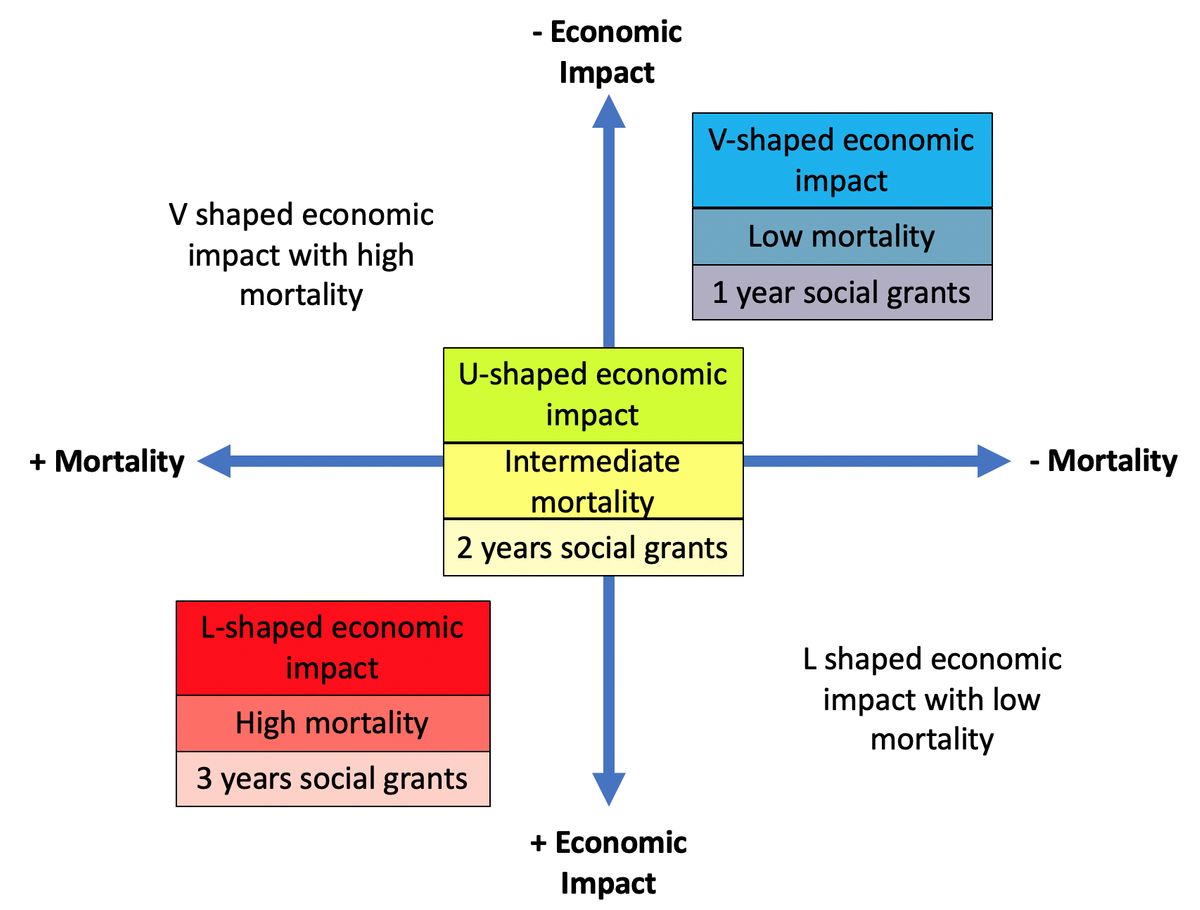
The conceptual framing that informed the choice of scenarios is presented in Chart 1. Importantly, the three COVID-19 scenarios developed for the project do not purport to present possible extreme outcomes, but rather consist of three reasonable alternatives — namely V-, U- and L-shaped scenarios, using the letter in the alphabet that most closely resembles the anticipated shape of the GDP growth curve. Each scenario consists of a set of three interventions in the IFs forecasting system that relate to economic growth, additional mortality and additional social grants.
The interventions are made in 2020 for the V scenario, in 2020 and 2021 in the U scenario and from 2020 to 2022 in the L scenario. The subsequent forecasts are generated by IFs.
The adjustments made within IFs for each scenario are summarised in Chart 4 and detailed in Annex C.
Chart 4: Interventions and assumptions
|
Scenario |
Economic growth |
Additional mortality due to respiratory infections |
Additional social transfers |
|
Reference scenario |
IMF global growth forecast released in October 2019. Global growth forecast at 1.4% in 2020. |
None |
None |
|
V |
IMF growth forecast released in April and June 2020. Includes sharp downturn in 2020 and rapid recovery in 2021. Global growth forecast at -4.9% in 2020. |
344 000 additional respiratory communicable disease deaths in 2020. From Imperial College best-case suppression scenario. |
For 2020 only. Country data where available, continental average for rest. |
|
U |
Same as V but recovery in 2022. See Annex C for growth rates per country for 2021. |
897 000 additional respiratory communicable disease deaths in 2020 and 468 000 in 2021. |
2020 same as in V. Half of that in 2021. None in 2022. |
|
L |
Same as V but recovery in 2023. See Annex C for growth rates per country for 2021 and 2022. |
1 450 000 additional respiratory communicable disease deaths in 2020, 886 000 in 2021 and 518 000 in 2022. The 2020 number is the Imperial College worst-case suppression scenario. |
2020 same as in V. Two-thirds in 2021 and one-third in 2022. None in 2023. |
Economic growth rates
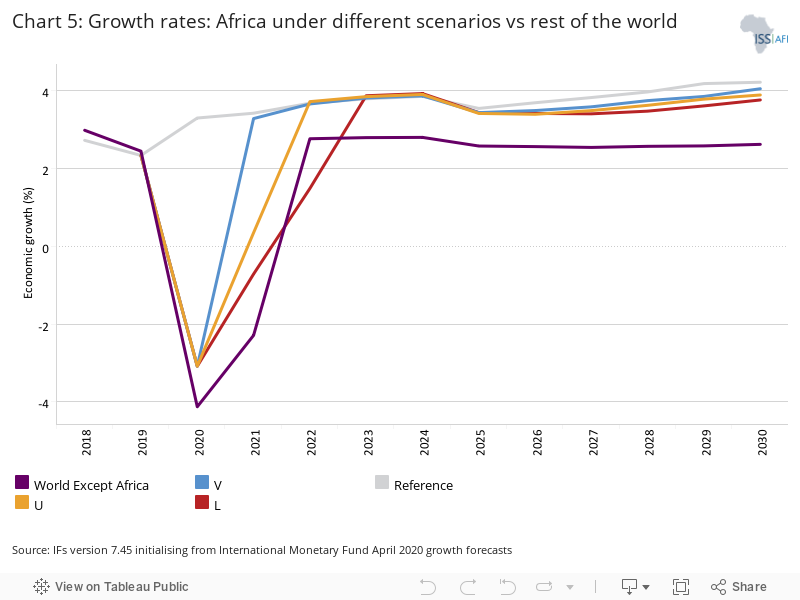
The IMF has twice updated its October 2019 growth forecasts. The first was in April 2020 and the second was at the end of June 2020. We use these updates as the basis for the V scenario. The V scenario is for an average growth rate of 3.1% for Africa to 2030 in the IFs forecasting platform, instead of the 3.8% reflected in the Reference or pre-COVID growth scenario. It includes a rapid economic recovery in 2021.
In the U scenario, Africa is only expected to recover by 2022; whereas in the L scenario recovery occurs in 2023, with significant long-term consequences discussed below. Chart 3 presents a comparison of the growth rates for each of the four scenarios as well as the anticipated average growth rate in the rest of the world. [13Note that the IMF October 2019 forecast is out to 2024. The forecast beyond that is from IFs.]
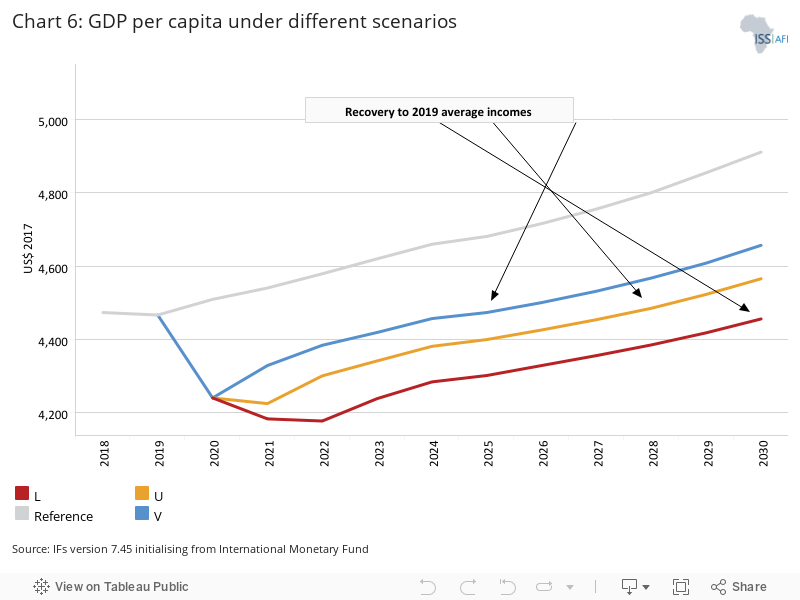
The economic contraction results in a large decline in GDP per capita, which can be used as a proximate measure for average incomes in Africa and is presented in Chart 6. From 2019 to 2020, GDP per capita in Africa, with its population of 1.3 billion, is expected to decline by about US$255 per person. In the V scenario, GDP per capita in Africa will recover to 2019 levels (US$4 466 per person) in 2024. In the L scenario that does not occur until 2030.
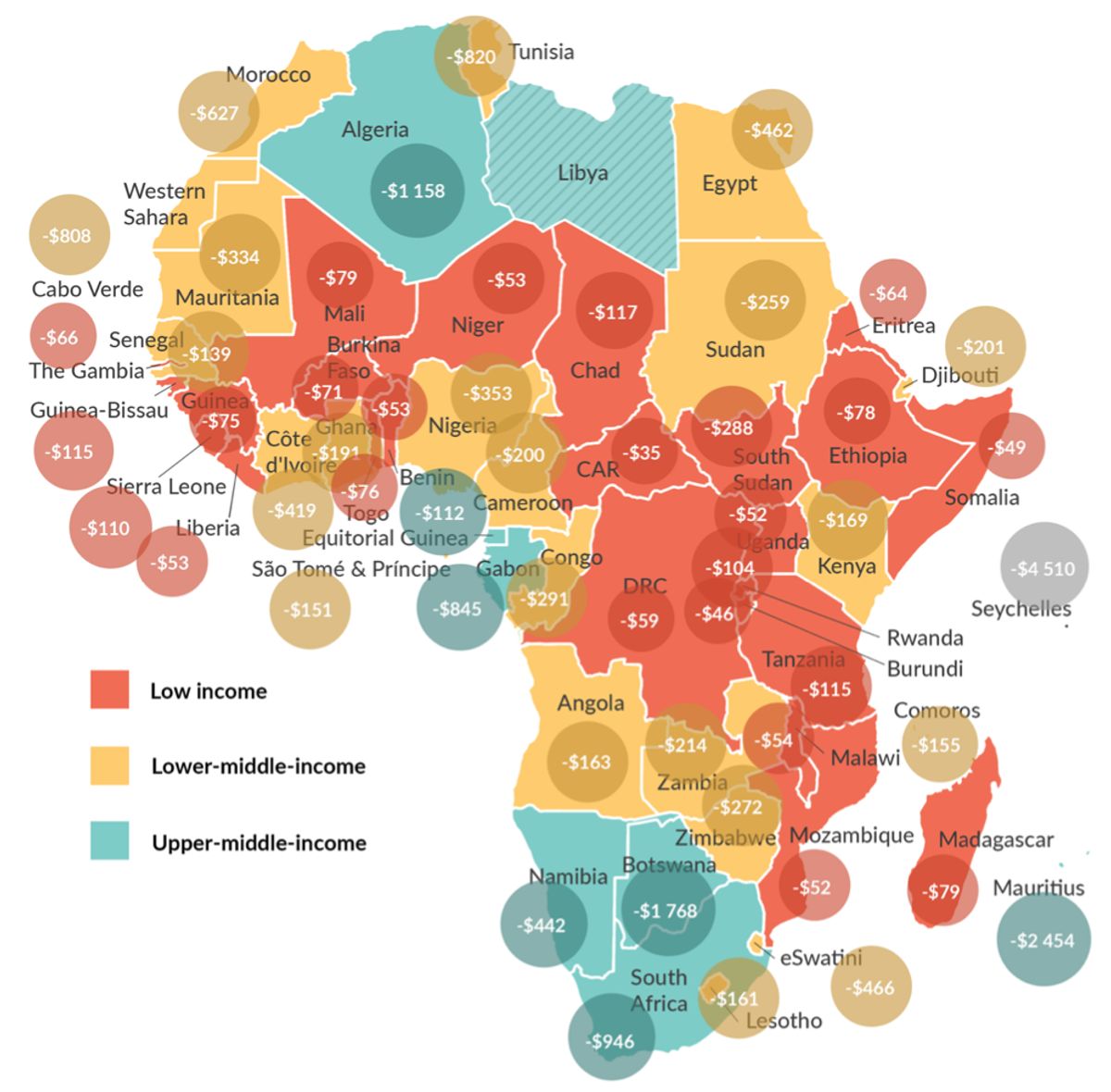
The 2020 contraction will be particularly severely felt in Africa’s six upper middle-income countries (excluding Libya) with a decline of US$1 115 from 2019 averages. For lower middle-income countries the average reduction is US$334 and for Africa’s 23 low-income countries the reduction is at US$48. Chart 7 presents the difference in GDP per capita in 2020 compared to 2019 for all African countries excluding Libya.
Infections and mortality
Forecasting rates of infection are particularly fraught for two reasons. Firstly, the low level of testing in Africa, in part due to initial problems with obtaining sufficient testing kits, undermined the availability of data. Africa has conducted about 1 700 tests per million people, compared to 37 000 tests per million in Italy and 30 000 per million in Britain. [14G Paravicini, All African countries now have coronavirus lab testing capacity - WHO chief, Reuters, 24 June 2020;
African countries move from COVID-19 readiness to response as many confirm cases, WHO]
Efforts are being made to scale up testing, and data is improving, but uncertainty remains about the actual rates of infection in many African countries. At the start of the outbreak only two countries in Africa could test for COVID-19. By the end of June 2020, all African countries had however developed laboratory capacity to test for the coronavirus. [15WHO, African countries move from COVID-19 readiness to response as many confirm cases]
Secondly, many young people display no or limited symptoms when infected, effectively carrying on with their lives, including going to work. As a result we consider that the impact on labour productivity and hence on economic growth is likely to be limited. This is because a large proportion of Africans are engaged in subsistence farming and the low-productivity service sector in the informal sector, which produce livelihoods but contribute little to national economic productivity.
Although Africa is at an early stage in the unfolding pandemic and data are incomplete, the continent is so far reporting very low mortality rates from COVID-19 infections. The most likely explanation seems to be that, at a median age below 20 years, the continent has a much younger population. This is a notable advantage since COVID-19 affects older people much more severely.
See Chart 8 for the population pyramid by age structure for Africa vs the rest of the world, where the median age is 34 years. There may be other explanations, such as cross-protection (limited immunity) conferred by exposure to other viruses with the result that when people get infected, they experience relatively mild symptoms. [16For a summary of thinking in this regard see L Spinney, Are we underestimating how many people are resistant to Covid-19?, The Guardian, 7 June 2020]
The most comprehensive forecast to date of the potential impact of COVID-19 is from Imperial College in London. Its March 2020 report, The Global Impact of COVID-19 and Strategies for Mitigation and Suppression, presents a number of scenarios ranging from no intervention to aggressive mitigation and suppression. In its best-case mitigation scenario it forecasts 122 million infections and 344 145 deaths in Africa, and in the worst case 515 million infections and 1 449 940 deaths.
On 7 May 2020 the WHO released its worst-case COVID-19 forecast of mortality in Africa. It noted that a relatively modest number of between 83 000 and 190 000 people in the WHO region of Africa [17This includes 47 African countries with roughly one billion people, excluding Djibouti, Egypt, Libya, Morocco, Somalia, Sudan and Tunisia.] could die of COVID-19. It estimated that 29 million to 44 million could get infected in the first year of the pandemic if containment measures fail. [18JW Cabore et al, The potential effects of widespread community transmission of SARS-CoV-2 infection in the World Health Organization African Region: A predictive model, BMJ Global Health, 2020.]
By comparison, about 700 000 Africans die annually from Aids and slightly fewer from malaria. COVID-19 is thus expected to have a relatively low mortality impact compared to these diseases.
Africa’s youthful advantage may, however, be undermined by two factors, both mentioned but not modelled in the Imperial College report. The first is its high levels of comorbidity, i.e. the extent to which Africans also suffer from other diseases or conditions such as diabetes, cardiovascular-related illnesses like hypertension, chronic kidney disease, HIV/Aids and tuberculosis. [19K Alcorn, People with HIV at greater risk of COVID-19 death in South African study, NAMAidsmap, 10 June 2020] The second is the lower capacity of health systems in Africa compared to elsewhere.
A recent study by the Center for Global Development found that once the rate at which infected people die from COVID-19 (the infection fatality rate or IFR) is adjusted for Africa’s high burden of comorbidity and low health system capacity, it ‘greatly diminishes, but does not entirely erase, the demographic-based advantage predicted in the lowest income setting.’ [20S Ghisolfi et al, Predicted COVID-19 Fatality Rates Based on Age, Sex, Comorbidities, and Health System Capacity, Center for Global Development, Working Paper 535, 12 June 2020, 2]
Significantly, whereas comorbidities are concentrated among the elderly in rich countries, in some developing countries such as South Africa a higher share is found among middle-aged people. [21J Sandefur et al, Predicting COVID-19 Infection Fatality Rates Around the World, Center for Global Development, 12 June 2020]
The WHO worst-case forecast of 190 000 deaths in 2020 is therefore significantly more optimistic than that from Imperial College which is, in turn, much more optimistic than the most recent study by the Center for Global Development, although the latter only compares ratios and does not provide absolute numbers. [22According to the WHO: ‘The new estimates are based on modifying the risk of transmission and disease severity by variables specific to each country in order to adjust for the unique nature of the region. The model predicts the observed slower rate of transmission, lower age of people with severe disease and lower mortality rates compared to what is seen in the most affected countries in the rest of the world. This is largely driven by social and environmental factors slowing the transmission, and a younger population that has benefited from the control of communicable diseases such as HIV and tuberculosis to reduce possible vulnerabilities.’ Smaller African countries alongside Algeria, South Africa and Cameroon were at high risk if containment measures were not prioritised, the WHO noted. The WHO study looked at 47 countries in the WHO African Region with a total population of one billion whereas the other studies were on all of Africa. WHO, New WHO estimates: Up to 190 000 people could die of COVID-19 in Africa if not controlled, COVID-19, 7 May 2020]
These three studies provide a range of best- to worst-case infections and mortality. xBy way of illustration, Chart 9 is taken from an accompanying blog done by the Center for Global Development and compares the predicted COVID-19 infection fatality rates for five African countries across the three studies.
For the purposes of this study, we adopt the best- and worst-case suppression scenario numbers from Imperial College as a basis for our mortality forecast. It is important to recognise that these are modelled forecasts, none of which have factored in the potential impact of new medicines (such as dexamethasone) or new treatments.
Whereas the growth forecasts for the various scenarios are done at a country level, the mortality forecast from Imperial College is applied as an intervention at the continental level, relying on the IFs system to allocate the mortality to individual countries through its data preprocessor. [23Modelling done by a consortium from three universities in South Africa considers a likely total 2020 mortality of between 34 015 and 49 774 in that country by November 2020. L López González, Read South Africa’s national, provincial COVID-19 projections in full, Bhekisisa Centre for Health Journalism, 20 May 2020. The additional respiratory infection for South Africa in our modelling for the V scenario is 16 610, in the U scenario it is 43 740 and in the L scenario it is 70 340 for 2020.]
The modelling done by Imperial College estimates that the 344 145 additional deaths from COVID-19 (used in the V scenario) would imply 122 million infected people and that the 1 449 940 additional deaths (used in the L scenario) would imply 515 million infected people, i.e. almost half of Africa’s total population. Given Africa’s large population, the mortality numbers, while serious, have a negligible impact on labour productivity and hence on GDP growth.
The vast majority of infected people would show no or light symptoms and as such we have not sought to forecast the impact on GDP growth. By contrast, UNECA, in its COVID-19 modelling released in April 2020, attributes substantial importance to reduced labour productivity as a key driver of economic growth, resulting in growth forecasts for 2020 of 1.8%, 0.1% and -2.6%. [24UNECA, COVID-19 in Africa: Protecting Lives and Economies in Africa, April 2020, 8. UNECA relied on the Imperial College infection and mortality results and modelled three scenarios at the continental level.] Our average 2020 growth rate for Africa, taken from the IMF, is at -3%.
In Guinea, Liberia and Sierra Leone more people died as a result of the indirect impact of Ebola from 2014 to 2016 than the combined official death toll of 11 325. [252014–2016 Ebola Outbreak in West Africa, Centers for Disease Control and Prevention, 8 March 2019] Given the economic impact of COVID-19, it initially appeared reasonable to expect that the indirect mortality effects of the pandemic would also outpace direct deaths from the disease, as was the case with Ebola.
Among the many reasons for the larger size of indirect mortality with Ebola is that it had the effect of channelling resources away from other government services and basic healthcare, resulting in an increase in malaria, HIV/Aids and tuberculosis, and other diseases. Maternal mortality rates typically increased by 75% as the number of women giving birth in hospitals and health clinics dropped. [26S Davies and B Bennett, A Gendered Human Rights Analysis of Ebola and Zika: Locating Gender in Global Health Emergencies, International Affairs, 92:5, 2016, 1041–60, reported in J Smith, Overcoming the ‘Tyranny of the Urgent’: Integrating Gender into Disease Outbreak Preparedness and Response, Gender & Development, 27:2.]
|
Chart 10: Learning from Ebola to combat COVID-19 in the Eastern DR Congo ‘Yet in some ways, Goma is more prepared than many other places in the world. Due to the Ebola crisis, the city is dotted with checkpoints where everybody is subjected to a temperature check — performed with handheld infrared thermometers — and required to wash their hands at chlorinated water stations before being allowed to pass. The city’s airport has an isolation chamber that was built for people displaying symptoms of Ebola but will now also be used for COVID-19. Now a modern laboratory is being constructed in central Goma to analyse coronavirus test samples from across eastern Congo.’ https://pulitzercenter.org/reporting/african-city-has-endured-war-and-ebola-now-comes-coronavirus |
Early in May, the WHO and the Joint United Nations Programme on HIV/Aids together issued a statement [27Joint United Nations Programme on HIV/AIDS (UNAIDS), The cost of inaction: COVID-19-related service disruptions could cause hundreds of thousands of extra deaths from HIV, 11 May 2020] expressing their concern that the number of deaths from Aids-related illnesses in sub-Saharan Africa could double if the provision of healthcare to people living with HIV was interrupted as a result of supply chain disruption, or health services being overwhelmed by the COVID-19 pandemic.
They noted that a six-month disruption of antiretroviral therapy due to the pandemic could lead to more than 500 000 extra deaths in the region in 2020-2021. The two agencies noted that in 2018 an estimated 470 000 people died of Aids-related deaths in sub-Saharan Africa.
Our findings, based on the mortality numbers from Imperial College, indicate a likely different pattern with COVID-19 to that with Ebola.
The additional mortality associated with each scenario compared to the Reference scenario is presented on a common scale in Chart 11. The bar graph makes a distinction between additional respiratory deaths (that include COVID-19 deaths) and additional mortality from other communicable diseases, malaria and other non-communicable diseases.
Beyond 2020 (V scenario), 2021 (U scenario) and 2022 (L scenario) all additional mortality should be viewed as a function of the reduction in health expenditure discussed in the next section, and not directly from COVID-19.
Source: IFs v7.45 initialising from the Global Burden of Disease from the Institute of Health Metrics and Evaluation. Within the IFs forecasting system we model the increases in mortality due to COVID-19 as the result of respiratory infections.
Note: The intervention applied in IFs and based on that done by Imperial College is as follows: V – 350 000 additional deaths in 2020; U – 900 000 additional deaths in 2020 and 470 000 in 2021; L – 1 450 000 deaths in 2020, 990 000 in 2021 and 520 000 in 2021.
Contrary to the experience with Ebola, Chart 11 would indicate that the direct mortality impact of COVID-19 from 2020 to 2030 (as estimated by Imperial College) would exceed the indirect mortality impact in the V scenario, that they are roughly equivalent in the U scenario and that, in the L scenario, direct mortality exceeds indirect mortality. [28Total additional mortality for V over the period 2020 to 2030 is 1 834 700 deaths, of which 642 300 are from respiratory infections. The numbers for U are 3 280 800 and 1 757 200. The numbers for L are 5 278 300 and 3 428 500.]
On the basis of that logic, and to avert a worst-case scenario, it would appear that decisions by most African governments to institute various measures related to lockdown, travel restrictions and social distancing, were appropriate. Effective treatments such as the recent findings relating to the steroid dexamethasone were not considered by Imperial College and would, of course, impact upon these forecasts.
Given challenges such as very low levels of testing to determine levels of infection, eventually a methodology based on excess deaths would probably yield the most useful insights into the true impact of COVID-19 in Africa. [29For an explanation and illustration of the associated methodology, see: US National Center for Health Statistics, Excess Deaths Associated with COVID-19, 2020]
An example of the problems inherent in reliance on testing to determine infections and mortality has been widely reported in respect of the northern Nigerian city of Kano, the second largest in the country. The state was in lockdown in April when gravediggers raised concerns that they were burying a higher than usual number of bodies.
Although the state governor issued a statement saying the deaths were unrelated to COVID-19, Nigerian President Muhammadu Buhari sent a team to investigate, as did the WHO. In May 2020 it became clear that the cause was indeed COVID-19 and not hypertension, diabetes, meningitis or acute malaria as claimed by the state government. Kano is just one of a number of emerging COVID-19 hotspots in Africa. Others include Cape Town, Djibouti and Mogadishu. [30R Maclean, Covid-19 outbreak in Nigeria is just one of Africa’s alarming hot spots, New York Times, 17 May 2020. In 2017, during an evaluation of its capacity to prevent, detect and respond to public health risks, Nigeria had scored poorly in both prevention and response. See S Dixit, Y Ogundeji and O Onwujekwe, How well has Nigeria responded to COVID-19?, 2 July 2020]
Excess deaths are typically defined as the difference between the observed number of deaths in specific time periods and the expected number of deaths in the same period. If the data obtained in this manner is sufficiently granular, it may be possible to get to a much more realistic picture of the true impact of COVID-19 that includes direct and indirect deaths. A recent study by EuroMOMO of excess deaths in 24 European countries all of which have more healthcare capacity than African countries suggests that there were about 170 000 excess deaths in a 10-week period from mid-March to the end May 2020. The discrepancy will surely be larger in most African countries. [31Tracking covid-19 excess deaths across countries, The Economist, 13 June 2020]
Revenue reductions and resource constraints
Africa has very limited capacity to respond to COVID-19 for reasons including low tax-to-GDP ratios and high debt levels. UNECA estimates that the continent’s response to the pandemic is at a mere 0.5% of GDP (US$44.7 billion). Half of that came from just two countries — South Africa and Egypt. [32Center for Global Development, UNECA executive secretary Vera Songwe in conversation with Masood Ahmed, 17 June 2020]
When UNECA published its report COVID-19 in Africa: Protecting Lives and Economies, in April 2020, it exposed the continent’s limited fiscal capacity. Africa’s tax-to-GDP ratio is low and declining. [33The tax-to-GDP ratio in Africa is the lowest of any region globally at 13.4% in 2018, compared to 14% in Asia, 25% in Europe, and 18% in Latin America. ] As borders closed and trade slowed in response to the pandemic, governments were collecting significantly less revenue.
The continent also has a high debt burden, spending roughly US$40bn annually on servicing its debt, in part because costs of borrowing are extremely high. Finally, the depreciation of many major African currencies since the beginning of 2020 has increased debt costs since bonds are issued in dollars and euros. [34Center for Global Development, UNECA executive secretary Vera Songwe in conversation with Masood Ahmed, 17 June 2020; P Madden, Figures of the week: Africa’s fiscal response to COVID-19, 13 May 2020]
Government revenues in Africa in 2020 are estimated at US$53 billion below the pre-COVID forecast for that year. The calculation from IFs is that public and private health expenditure will decline by US$4.4 billion in 2020 in all three of our COVID-19 scenarios. Thereafter, the reductions differ in accordance with the annual growth rate for each scenario.
By 2030, the cumulative reduction in health expenditure on the continent is forecast to be US$135 billion less in the V scenario compared to the Reference scenario, US$188 billion less in the U scenario and US$233 billion less in the L scenario. There are, of course, huge variations in how countries are reacting to the pandemic. [35For a summary of country-level responses see: IMF, Policy Responses to COVID] Some may protect their health spending, reallocating expenditure from other budget lines to health. Even within the health budget funds may be reallocated from other non-communicable disease treatment to measures that respond directly to COVID-19.
By 2030, COVID-19-related mortality would result in 2.1 million additional deaths in the V scenario, 3.6 million in the U scenario and 5.8 million in the L scenario, including both direct and indirect mortality
Additional social grants
A third and final intervention within the IFs forecasting platform relates to efforts by African governments to cushion the economic impact of lockdowns and other COVID-19 containment measures through additional social grants, food parcels and the like.
Here we gathered country-level data where it was available or applied an average in 2020 where we could not find country-level data, and then scaled these amounts back in 2021 (for the U scenario) and to 2022 (in the L scenario).
The impact is that 3.4 million fewer Africans are classified as extremely poor in 2020 than would have been the case without the additional transfers and slightly fewer in 2021 (in the U scenario) and in 2022 (in the L scenario). [36Equivalent to 0.05 percentage points.]
Summary impact
Chart 13 provides a summary of the impact of COVID-19 on changes in poverty, average GDP per capita, additional deaths and size of the economy.
The forecast taken from the IFs model is that debt is expected to increase by about 5 percentage points of GDP in 2020 compared to the Reference scenario. In the worst case, the L scenario, debt is likely to increase by about nine percentage points of GDP by 2022 compared to the Reference scenario.
The impact of additional social grants to offset the impact of COVID-19 is to marginally reduceinequality as measured using the Gini index. But once these fall away, inequality increases and reverts to the 2019 average only several years later.
Net aid receipts in Africa are likely to decrease in 2020 (or 2021 given that current budgets are probably set) when compared to 2019 since the economies of donor countries are expected to contract. Thereafter, aid will probably resume its slow increase in absolute numbers, consistent with the historical trend.
However, because of the large contraction in the economies of Africa, the importance of aid as measured in its contribution to GDP and to government revenues will in all likelihood increase. Africa will, for several years, become more and not less dependent on aid. Because most aid flows to low-income countries, these countries will experience a large decline in aid receipts to the extent that aid may also decline in its contribution to GDP.
Impact on key SDG targets and goals
The short-term impact of COVID-19 on extreme poverty is particularly severe, given the large economic growth shock in 2020. When compared to the pre-COVID-19 trajectory, an additional 14 million more Africans will live at incomes below the US$1.90 extreme poverty threshold in 2020 alone.
In the V, U and L scenarios, in 2021 an additional 25 million, 29 million or 30 million Africans respectively would drop below US$1.90 per person per day compared to the pre-COVID-19 poverty forecast. The country-level estimates for the pre-COVID-19, V, U and L scenarios for 2019 (pre-COVID-19), 2020, 2025 and 2030 are in Annex B.
Although it has been evident for several years that Africa will miss the headline SDG goal of eliminating extreme poverty by 2030 [37J Moyer and S Hedden, Are we on the right path to achieve the sustainable development goals? World Development, Volume 127, March 2020], the impact of COVID-19 is set to widen the gap. Our findings are slightly more optimistic than those of the World Bank. [38According to the World Bank: ‘The 2020 downturn will likely increase the SSA poverty rate by at least 2 percentage points. This would mean that an additional 26 million people in SSA would fall into extreme poverty (defined as those living under US$1.90 per day in 2011 PPP). This projected increase in the poverty rate would return SSA to 2015 poverty levels, effectively wiping out 5 years of progress reducing impoverishment.’ J Montes et al, Poverty & Equity Notes, World Bank Group, Number 20, May 2020, 3.]
The impact of the three scenarios on extreme poverty at the continental level is presented in Chart 14. Whereas roughly 570 million Africans (33% of total population) would probably still live in extreme income poverty in 2030 in the Reference scenario, the impact of COVID-19 is to increase that number to 607 million (V scenario), 621 million (U scenario) or 640 million (L scenario), ranging from 35.7% to 37.6% of the total population.
Before COVID-19, in the Reference scenario, extreme poverty in Africa would have declined by 2.5 percentage points from 2019 to 2030; equivalent to an increase of 101 million people given Africa’s rapid population growth. [39Africa’s population is currently at 1.343 billion and should increase to 1.710 billion by 2030.]
In the V scenario extreme poverty will only decline by 0.6 percentage points (an increase of 138 million people). In the U and L scenarios, the per cent of extremely poor Africans will actually increase above the 2019 rate (reflecting an increase of 152 million and 171 million people respectively), reflected in Chart 14.
The countries that are most negatively affected under all three scenarios are Nigeria, the DR Congo, Ethiopia, Niger and Tanzania. Nigeria and Ethiopia are the two most populous countries in Africa while the DR Congo and Tanzania rank fourth and fifth respectively. Niger on the other hand has the most youthful population on the continent (at a median age below 16 years) with some of the lowest human development indicators, which would probably deteriorate even further.
Annex C presents a summary of progress towards selected SDG goals and targets by 2030 under each of the four scenarios. Africa is already projected to miss most of the SDG targets and the impact of COVID-19 is set to further constrain progress. For example, whereas the percentage of Africa’s undernourished population would have modestly declined to 221 million people (or 13% of total population) by 2030 in the Reference scenario, it is now set to increase. [40To 233 million, 239 million or 247 million in the V-, U- and L scenarios respectively.] Infant mortality will, by 2030, be three times higher than the target set by the UN.
Although Africa is making good progress in primary education enrolment, primary education completion rates are more than 10 percentage points below the target. Secondary and tertiary enrolment and completion rates are significantly off track. While in 2030 Africa was expected to achieve an upper secondary education graduation rate of 40% (compared to the SDG target of 97%), the impact of COVID-19 will reduce progress by two percentage points.
Access to improved water infrastructure, essential to combat COVID-19, would have improved to 83% by 2030. However, that too is likely to reduce by at least a percentage point. The associated SDG target is 98% access.
Given the many unknowns about the virus, governments have to make decisions based on incomplete facts and information at their disposal. This requires a balance between the deleterious economic repercussions and the potential human suffering from COVID-19.
Initially, states with more developed economies, such as Algeria, South Africa, Kenya and Egypt, which are more exposed to global interaction through trade and tourism, experienced the largest infection and fatality burden. Comparatively, countries with low levels of economic development (and hence more limited interaction globally) and high levels of dependence on subsistence farming, such as Sierra Leone and Malawi, appear to have much lower rates of infection and mortality. This divergent trend is, however, unlikely to continue as rates of community transmission accelerate.
While rates of infection and mortality differ widely from country to country, all of Africa has been severely affected by the economic downturn. This is especially so for large energy exporters such as Algeria, Angola and Nigeria, and in the case of Egypt, due to the impact of reduced global trade and income from the Suez Canal.
Having bought time for the preparation of their health systems, most countries are now easing restrictions in order to restore their economies. A number, including South Africa, are implementing so-called risk-adjusted (or more targeted) post-lockdown strategies, including potentially isolating vulnerable groups and regionally differentiated responses. These efforts are accompanied by mass testing coupled with contact tracing while awaiting improved treatment (such as dexamethasone) and eventually a vaccine.
From health crisis to economic and human development crisis
The restriction of economic and social activity has meant that COVID-19 has become a systemic human development crisis in Africa.
After lockdowns in Africa are lifted, the economic recovery is likely to be gradual, worsened by a collapse in tax revenues and a notable reduction in employment levels and household incomes. Certain sectors such as tourism — on which numerous African countries depend heavily for foreign currency — may take several years to recover. Prospects for tourism have been downgraded several times with current estimates by the World Tourism Organization pointing to a decline of 58% to 78% in tourist arrivals for 2020. [41UN World Tourism Organization, International Tourism and COVID-19]
The further challenge of a second or third wave of infections poses additional risks to Africa’s recovery. Developments in Europe and North America will need to be watched closely as these countries go into their autumn and winter flu season.
On the upside, there is some indication that COVID-19 may accelerate technology adoption and the transition to a digital economy, and even facilitate a degree of leapfrogging towards a more sustainable economy fuelled by renewable energy. Coming off a low technology and ICT base, COVID-19 has some potential to accelerate Africa’s economic diversification and speed up digitisation as domestic businesses seek to operate while mitigating risks, establishing new work practices and cultures in the process.
In an effort to mitigate the economic impact, many African governments are resorting to social transfers, credit guarantees and monetary easing, but the fiscal space available for such efforts is limited. In addition to borrowing more money, governments are inevitably revising their budgets to bring spending (such as on public sector wages and on interest) in line with the very evident economic contraction and expectation of reduced revenues.
Economic contraction is further compounded by high levels of debt in many African countries. Levels of indebtedness have steadily increased in recent years and the collapse in growth due to COVID-19 is thus likely to trigger a debt crisis and potentially even a default in some instances. Lower borrowing capacity means countries also have less capacity to prevent and mitigate the impact of the pandemic, and this will in all likelihood result in more deaths.
Countries such as Angola and Nigeria that are largely dependent on oil revenues have been hit particularly hard as prices collapsed with the global reduction in demand. Revenue from remittances [42According to the World Bank, global remittances would experience the sharpest decline in recent history, falling by one fifth in 2020. Its forecast for sub-Saharan Africa is a decline of 23.1% in 2020 and a decline of 19.6% in North Africa and the Middle East. The outlook for 2021 is uncertain, but the World Bank expects a recovery of 4% in sub-Saharan Africa and 1.6% in North Africa. World Bank Group, World Bank predicts sharpest decline of remittances in recent history, 22 April 2020.] will also decline as the diaspora has less money to send home. Fewer remittances would represent a loss of a crucial financing lifeline for many vulnerable households in Africa.
Finally, COVID-19 is unfolding at a time of unprecedented shifts in power, influence and economics — trends that have reduced global cooperation and multilateralism deemed essential to combat the pandemic. The manner in which these shifts play out in Africa, in relation to the trade and diplomatic relations of African states with emerging regional blocs such as Southeast Asia, will probably shape the trajectory of Africa’s regions in marked ways. This is especially true in relation to lending, infrastructure, industrial development and trade.
Africa has not been asleep at the wheel. In addition to country-level efforts, the African Union (AU) has established the Africa COVID-19 Response Fund, appointed AU COVID-19 Special Envoys to support resource mobilisation, and is seeking postponement of debt repayment and in some cases debt cancellation.
It has established an Africa Centres for Disease Control and Prevention (CDC)-led initiative for pool procurement and distribution of pharmaceutical products and health equipment to member states, and created ministerial-level task forces on health, finance, transport, trade and industries. [43Report on the coordination meeting of the African Union Development Agency (AUDA-NEPAD) with the AU Regional Economic Communities (RECs) under the patronage of the chairperson of the African Union Commission (AUC): The Regional Response to COVID-19 held on 18 May 2020, 3.]
In June 2020, AU chairperson Cyril Ramaphosa launched the Africa Medical Supplies Platform as a single online marketplace to enable the supply of COVID-19-related critical medical equipment in Africa. A summit on COVID-19 responses with China was also hosted.
Beyond the emergency policies to fight the pandemic and mitigate its associated short-term economic impact, there is an obvious need for policies to build future resilience and improve long-term growth prospects. To this end, four strategic priorities flow from our analysis of the COVID-19 crisis.
The first, and most urgent, is effective responses to Africa’s emerging debt crisis. The second relates to the importance of increased and more effective health spending if the continent is to effectively respond to future pandemics. Third is the provision of safe water, improved sanitation and other basic infrastructure — something that Africa in general has underinvested in. The final policy priority is the necessity of spurring Africa’s economic transformation to boost much more rapid and inclusive economic growth and compensate for the impact of COVID-19.
Debt
Concerns about Africa’s increased debt levels have been growing for several years fuelled, in part, by large loans for infrastructure by countries such as Angola, Kenya and Ethiopia. Many countries have also shifted from concessional multilateral creditors such as the IMF and the World Bank to non-concessional debt on the commercial market with higher interest rates, lower maturities and higher refinancing risks.
In addition to pre-COVID-19 rising debt levels, African countries are now also borrowing additional funds to ameliorate the immediate impact of the pandemic such as for business relief and to provide social grants to the poor.
Whereas a debt burden of 70% of the GDP may not be a problem for an economy growing at 6%–7% per annum, it suddenly becomes a very large problem when growth rates decline to 2%–3% and that money is linked to commercial rates. Most countries on the continent also pay a premium based on perceptions of higher risk in Africa. The continent pays 5%–6% interest on 10-year government bonds compared to near zero in Europe and America. [44M Mutize, African countries aren’t borrowing too much: They’re paying too much for debt, The Conversation, 19 February 2020]
COVID-19 now probably means a debt crisis and may even serve as a tipping point that could see a return to some of the requirements associated with the establishment of the Heavily Indebted Poor Countries (HIPC) initiative by the World Bank and the IMF in 1996. HIPC provided debt relief and reduced debt service payments of up to 80% for eligible countries. [45C Onyekwena and MA Ekeruche, Is a debt crisis looming in Africa?, 10 April 2019] It saw, for the first time in their history, the IMF and the World Bank writing off their own debt.
For example, Sudan is at risk of relapsing into political instability and potential conflict. The impending crisis saw Sudanese Prime Minister Abdalla Hamdok write to the UN Secretary-General, indicating that COVID-19 poses ‘profound challenges’ to the country’s health system, economy, and society as a whole. He asked for financial and technical support to tackle the pandemic. [46UN, Sudan: Coronavirus could be tipping point for ‘untold suffering’, Bachelet urges sanctions relief, UN News, 28 April 2020]
The question is where to find additional financial means to respond to the crisis. Inevitably, the first option is to look in national budgets, including the amounts spent on debt payments which are generally larger, as a portion of the GDP, than that spent on health.
In Kenya, when the 2020/2021 budget report was presented to its National Assembly, it revealed that of the US$15 billion total projected revenue collection, US$8.5 billion (56%) would go to repayments on the country’s US$58 billion debt. [47J Mutua, SGR services at risk over Sh38bn China firm debt, 10 June 2020] At this level, debt repayments squeeze out social investments and undermine the fight against poverty and inequality.
According to the IMF, Africa would need an estimated US$114 billion in 2020 to manage the coronavirus. [48K Georgieva, Opening Remarks at High-Level Virtual Event on ‘Mobilizing with Africa’, 17 April 2020] Albert Zeufack, Chief Economist for Africa at the World Bank, stated that: ‘Africa alone will not be able to contain the disease and its impacts on its own; there is urgent need for temporary official bilateral debt relief to help combat the pandemic while preserving macroeconomic stability in the region.’ [49The World Bank, For Sub-Saharan Africa, Coronavirus Crisis Calls for Policies for Greater Resilience, April 2020]
In addition to the Republic of Congo, Mozambique, Somalia, South Sudan and São Tomé and Príncipe that are already all in debt distress, Burundi, Cape Verde, Cameroon, Central African Republic, Chad, Djibouti, Ethiopia, The Gambia, Ghana, Kenya, Malawi, Mauritania, Liberia, Sierra Leone, Togo and Zambia are at high risk of debt distress. [50The World Bank, COVID-19: Debt Service Suspension Initiative, 29 June 2020]
As the depth of the crisis becomes evident, the initial calls for a standstill are shifting to debt forgiveness and cancellation, including by China that operates bilaterally, outside of the Paris Club, and where contractual details are opaque. China is now the biggest bilateral creditor of Africa and is owed some US$145 billion.
To supplement measures towards better revenue management, including from taxes, the World Bank now calls for adherence to five key principles to improve debt transparency and improve investment flows: [51D Malpass, Debt and investment transparency for better outcomes, World Bank blogs, 19 June 2020]
- Spell out loan contract terms and payment schedules
- Full disclosure of the stock of public and publicly guaranteed debt, State Owned Enterprise liabilities, and debt-like instruments
- Enable borrowers to seek relief from excessive confidentiality clauses so they can proceed with more transparent data reporting
- Promote effective and prudent use of collateral and liens in sovereign borrowing; and
- Insist that borrowers and lenders avoid violations of legal requirements of other creditors, such as negative pledge clauses.
At the G20 summit in April 2020, Africa called for a two-year debt standstill on all principal debt and interest payments to see if rebuilding and growth would resume. The G20 countries subsequently agreed on a limited standstill on bilateral payments that would postpone approximately US$11.53 billion of payments due by poor countries this year, well short of the US$44 billion debt relief that the AU envoys and African finance ministers are seeking.
Globally, 73 countries are eligible for relief under the Debt Service Suspension Initiative (DSSI) although some, such as Ghana that are at high risk of distress, are not participating in the initiative since opting for the relief could negatively affect the cost of existing loans from private lenders. [52This is through the Debt Service Suspension Initiative, T Maeko, Manuel: African nations need $40bn for debt relief, Mail & Guardian, 19 June 2020]
In addition, Africans have called for the allocation of more IMF Special Drawing Rights to help withstand the shocks caused by the pandemic. China subsequently joined the G20 plan for a temporary freeze on bilateral debt repayments, but it does not deal with private bondholder debt which makes up almost one-third of Africa’s total debt load. [53C van Staden, Not much give from China in its relationship with Africa, Daily Maverick, 28 June 2020]
Support from institutions such as the World Bank and the IMF are encouraging. However, as a recent blog by the Center for Global Development notes,[54S Morris, C Landers and A Gardner, More World Bank borrowers will need grants, not loans. as a result, more world bank donors will need to pony up, Center for Global Development, 4 June 2020] more borrowers will need grants, not loans. In addition, it is necessary to adjust the terms of such assistance to promote the sustainability of debt and repayment. [55The World Bank, Debt Service Suspension and COVID-19, May 2020]
Health and health spending in Africa
The epidemics of Ebola, Zika and now the COVID-19 pandemic demonstrate the global significance of new emerging diseases with potentially catastrophic effects. Yet most African countries are spending below the 2001 Abuja Declaration target of allocating at least 15% of public revenue to health. [56See, for example: WHO, The Abuja Declaration: Ten Years On, 2011. Within IFs the following countries have government expenditure in excess of 15%: Eswatini, Malawi, The Gambia, Algeria, Lesotho, Republic of Congo, Ethiopia, São Tomé and Príncipe, Kenya, South Africa, Cape Verde, Niger, Rwanda and Zambia; Y Adegoke, African economies are spending up to five times their health budgets on debt repayments, QuartzAfrica, 30 April 2020] Many, such as Ethiopia, also rely on significant levels of external funding, which may decline in the current environment. The COVID-19 pandemic necessitates significant additional health financing to prepare for, respond to and treat the disease, never mind expenditure on other health priorities. [57For example, the Health Finance and Governance project that analysed 43 of sub-Saharan Africa’s health financing outlooks found that 13 had reached the internationally accepted target of US$60 per capita health spending. It projected that nine additional countries would reach this target by 2020 on the assumption that health expenditure would follow increases in economic growth. Health Finance and Governance, Universal Coverage of Essential Health Services in Sub-Saharan Africa: Projections of Domestic Resources, United States Agency for International Development (USAID), 2013]
Given the global economic slump, it is clear that African countries will struggle to even maintain current levels of health expenditure. [58Between 1.5% and 3% of GDP additional health financing is required to adequately respond to COVID-19 over a period of 250 days. In a Suppression scenario where wide-scale aggressive social distancing is pursued, an additional roughly US$23.54 billion would be required to prepare and treat the disease, and in a Social distancing scenario US$53 billion would be the target. P Schneider, F Pivodic and K Jison Yoo, How much health financing does Sub-Saharan Africa need to fight COVID-19 (coronavirus)?, World Bank Blogs, 15 April 2020] The COVID-19 pandemic could, like Ebola in West Africa, result in resources being channelled away from basic healthcare services. The limited funds for medical research and development in Africa may also decline. Governments must therefore ensure that their focus on COVID-19 does not result in an increase in malaria, HIV/AIDS and tuberculosis (TB), among others. They should also invest in the different technologies that can produce vaccines.
According to an Imperial College study: ‘Maintaining the most critical prevention activities and healthcare services for HIV, TB and malaria could significantly reduce the overall impact of the COVID-19 epidemic.’ [59AB Hogan et al, The Potential Impact of the COVID-19 Epidemic on HIV, TB and Malaria in Low- and Middle-Income Countries, Report 19, Imperial College London, 1 May 2020] The study found that ‘in high burden settings, HIV, TB and malaria related deaths over five years may be increased by up to 10%, 20% and 36%, respectively, compared to if there were no COVID-19 epidemic.’ [60AB Hogan et al, The Potential Impact of the COVID-19 Epidemic on HIV, TB and Malaria in Low- and Middle-Income Countries, Report 19, Imperial College London, 1 May 2020] Decreases in vaccination rates compounded these challenges.[61UNDP, Human Development Reports, COVID-19 and Human Development: Assessing the Crisis, Envisioning the Recovery, 2020, 12]
A sharp focus is also required on maternal mortality rates. These rates may easily increase as the number of women giving birth in hospitals and health clinics drops, due to concerns about being infected and a health system seized with other priorities.
Because of the various factors at play, it is crucial that Africa and its development partners carefully consider investments in the healthcare system. The emphasis should be on domestic resources and cost-effective management of existing funds.
Africa also needs to prepare for the eventual availability of a vaccine against the novel coronavirus. In 2020 there were more than 220 projects under way globally to develop an effective vaccine, 16 of which had entered clinical trials, and hope is growing for a breakthrough. [62WHO, Draft landscape of COVID-19 candidate vaccines, 24 June 2020]
But once medicine or a vaccine is available, the global demand could quickly outstrip supply and it is probable that populations in poor countries will struggle to access these treatments. As the continent most likely to be severely affected in this regard, African leaders should make their voices heard.
Africa must enhance its domestic research and development, and vaccine production capability to avoid remaining a net consumer that would prevent the continent being continuously dependent on external supplies. African countries with proven capacity must be encouraged to undertake domestic COVID-19 vaccine production using local isolates and well-established vaccine technologies. This is an area in which the AU and the Africa CDC should play an important role. [63United Nations Conference on Trade and Development, COVID-19 heightens need for pharmaceutical production in poor countries, 27 May 2020]
In response to growing awareness of the challenges in this regard, the European Union (EU) has secured nearly US$8 billion to help ensure universal and affordable access to COVID-19 medication, including supporting a ‘people’s vaccine’. On 19 May 2020, the World Health Assembly called for equitable access to vaccines and treatments against the virus. Then there are the various financial instruments by the global vaccine alliance Gavi aimed at incentivising vaccine manufacturers to produce sufficient quantities of COVID-19 vaccines, and to ensure access for developing countries. [64UNCTAC, COVID-19 heightens need for pharmaceutical production in poor countries, 27 May 2020. Also Gavi, Gavi launches innovative financing mechanism for access to COVID-19 vaccines]
The successful rollout of a vaccine in Africa would involve simultaneously navigating the complex interplay of poor health systems, the challenge of maintaining treatments of other diseases such as malaria, as well as managing insecurity and political instability. Countries such as Chad, Mali, the DR Congo, South Sudan and Somalia have limited infrastructure, weak political institutions, high burdens of poverty and large displaced communities that will complicate the delivery of a vaccine, in addition to their existing high disease burdens such as from malaria. [65Africa is home to 90% or 380 000 of all malaria deaths in 2018. See: E Sherrard-Smith et al, The Potential Public Health Impact of COVID-19 on Malaria in Africa, Report 18, Imperial College London, 1 May 2020]
Other important issues may also fall by the wayside such as limiting access to sexual and reproductive health and increasing gender-based violence. Given the importance of advancing Africa’s demographic dividend with all its attendant advantages, much greater efforts are required to roll out modern contraceptives and to use the COVID-19 pandemic to refocus Africa on the essentials of basic healthcare.
Among the measures required are:
- Adequate investment in preventive measures, including education and awareness campaigns around hand washing, social distancing and overall responsible behaviour by the general public.
- Adequate allocation of funds to public healthcare facilities where the majority of the population can access treatment.
- Greater investment in primary healthcare and capacity building for basic testing and diagnostics, particularly in rural areas.
- Creating a flexible operating framework to ensure adequate healthcare personnel through simplified hiring processes, including greater collaboration between public and private hospitals.
- Promoting better cooperation between national, sub-national and local authorities that engage to build on local knowledge and capacity, especially that acquired by countries that have experienced epidemics like Ebola.
- Creating disease and public health surveillance systems to systematically collect, analyse and monitor data to establish trends, and predict and minimise havoc from disease outbreaks.
- Agitating for better, transparent and efficient procurement systems. Africa is currently facing a shortage in testing equipment owing to global demand and competition. Having a united voice and action plan on a continental level could provide additional traction in this regard.
- Much greater transparency, with prioritised and efficient use of available resources, is necessary to ensure optimum results in combating the disease.
- Apart from greater integration of scientists into public policy debates, promoting innovation, use of technology and partnerships in medical research and infrastructure are crucial to cut costs.
- Re-engineering health systems in Africa to broader visions beyond COVID-19, to cater to specific needs of different groups of people in cities and rural areas.
- Generally strengthening governance in the health sector to improve the quality of health services.
- Finding ways to partner with private healthcare service providers to unlock their capacities, such as is occurring in South Africa.
- International support for the above via funding and technical support.
The next pandemic that Africa faces could be more deadly than COVID-19.
Poor levels of access to water, sanitation and hygiene (WaSH)
It is clear that Africa’s high communicable disease burden reflects and contributes to its lower levels of human development compared to other regions globally. Inadequate access to clean water, proper sanitation and hygiene is central to this burden.
It is therefore not surprising that Africa’s urban citizens have some of the lowest levels of access to basic services worldwide. In fact, access to modern medicine, rather than proper planning and water, sanitation and hygiene (WaSH) infrastructure, has been helping to keep epidemics and ill health at bay in much of urban Africa — until COVID-19 further underlined the deficit in basic infrastructure. [66TJ Bollyky, Plagues and the Paradox of Progress Why the World Is Getting Healthier in Worrisome Ways, Cambridge: MIT Press, 2018.]
Given the low levels of access to safe water, sanitation and hygiene services, Africa finds itself at a disadvantage in tackling the COVID-19 contagion. How does one undertake the most basic countermeasures, such as washing of hands, without access to clean water?
Poor access to WaSH is a well-established contributor to the global burden of disease that inhibits sustainable development, and which is complicated by rapid urbanisation. Urbanisation in Africa has seen the rapid growth of large informal settlements that do not have the basic infrastructure, such as safe water and waterborne sewage, to cope with the large influx of people on top of natural population growth. Many housing units are almost exclusively self-constructed and neighbourhoods are organised independently of the central governing authority.
Africa’s urban population is forecast to more than double by 2050, adding more than 800 million people to Africa’s cities. The UN Population Division anticipates that between 2018 and 2035, all ten of the world’s fastest growing cities will be in Africa and 21 will be in the top 30. [67UN Department of Economic and Social Affairs, Population Division, 2018] Twelve of these 30 cities are in West Africa, four of which are in Nigeria, and they will add about 200 million people to urban areas in Africa by 2050.
Hypothetically, the centralisation of service delivery points for water, sanitation and health in urban areas should make service delivery easier, compared to the challenge of rolling out healthcare or sanitation in sparsely populated rural areas. However, most of Africa’s cities arepoorly designed, already congested and growing rapidly.
Lack of adequate access to improved hygiene facilities and safe water are even more dire in rural areas. The implications are widespread and go beyond just facilitating the spread of communicable diseases and other health issues like malnutrition and stunting. Inadequate access to WaSH services in rural areas also aggravates existing social and gender inequalities. Women and girls in particular spend more time travelling long distances to fetch water. This not only predisposes them to greater risk of violence, but they are also forced to forego education.
The lack of access to safe water therefore impedes an effective response to COVID-19 in many countries and is compounded by the widespread practice of water sharing among households. Although there is currently no evidence that the virus can survive in drinking water, the act of water sharing or the need to fetch water can facilitate COVID-19 transmission through close interpersonal interactions. [68J Stoler, WE Jepson and A Wutich, Beyond Handwashing: Water Insecurity Undermines COVID-19 Response in Developing Areas, Journal of Global Health, 15 May 2020]
The lack of access to safe water in Africa, particularly in urban areas, is a function of poor management and outdated infrastructure that has not kept up with growing demands for WaSH services. In the short term, government bodies charged with management and delivery of water should ensure that:
- Clean water is delivered to people living in informal settlements on a regular basis, even if that is done by deploying water tankers.
- Portable sanitation services are provided at strategic points with regular cleaning services to maintain hygiene.
Where possible, hand sanitisers are provided to mitigate situations where people have limited access to water. A number of beer breweries and distilleries have shifted production to hand sanitisers, and this is a way in which governments could spur small-scale business while combating the virus. - Community awareness campaigns continue to encourage responsible behaviour and sensible individual decision making, even under difficult circumstances.
- Underground water is better used, through boreholes and wells.
For the long term, governments should promote:
- Conscientious engagement with the private sector, establishing public-private partnerships in order to ensure the delivery of WaSH infrastructure.
- Appropriate urban planning and design to enable real-time planning and scaling of urban services.
- Increased investments in water and sanitation to adequately account for current and projected needs of populations to 2030 and beyond. Africa currently invests just 0.5% of GDP in water and sanitation. [69F Ndaw, COVID-19: Solving Africa’s water crisis is more urgent than ever, April 2020]
- Better management strategies for dealing with water stress. This includes greater investment and capacity in wastewater treatment plants and reuse of wastewater.
- Investment in modern and locally available material for water distribution and sanitation facilities. The infrastructure in many African cities dates back to colonial times.
- Viable provision of water: many African countries can barely manage the costs of supplyand distribution of water despite often disproportionate fees. Others rely on unsustainable subsidies, making it difficult for the private sector to augment the limited offerings from the public sector.
- Educational and awareness campaigns about conservation of water to ensure consumers play their part in water management.
- Local and biodegradable technologies in sanitation facilities to ensure even rural communities get access to hygienic sanitation.
African countries should make WaSH part of their economic recovery, encourage community engagement and explore new and localised ways for service delivery. Modern technology can help overcome much of Africa’s basic infrastructure gap in poor urban and even rural communities. It can combine smart metering, pay-as-you-go, big data, geolocation and the internet of things to establish smart grids, solar home systems, map sanitation facilities, monitor decentralised water points, operate water ATMs in informal settlements, and manage waste flows.
Pay-as-you-go models allow low-income customers to make small incremental payments towards otherwise unaffordable goods and services including water and sanitation. The result is a sustainable business model able to respond to the challenges of the urban poor and urban poverty traps. [70See, for example: GSMA, Digital Solutions for the Urban Poor, 10 March 2020]
Need for economic transformation in Africa
This investigation into the impact of COVID-19 underlines the immense challenges that Africa faces in achieving the SDGs and realising the ambitions set out in the AU’s Agenda 2063 vision. Our forecast of a post-COVID-19 average economic growth rate of 2.6% (L scenario) to 3.2% (V scenario) is several times too low to change the continent’s development prospects to 2030. Much more robust and inclusive growth is required.
Once the immediate crisis has been contained, governments will have to work hard to claw back the ground lost due to the pandemic. This will include putting their countries back on a pathway towards debt sustainability. That will, in turn, require a renewed determination to implement revenue-mobilisation, debt-management and public financial reforms. Employment-intensive growth will require private-sector investment and a facilitating business environment.
Indeed, the COVID-19 pandemic underscores the importance of accelerating structural transformation in African economies towards much more rapid, sustainable and inclusive growth — while also illustrating some of the potential pathways that could accelerate that transition. [71J Cilliers, Africa First! Igniting a Growth Revolution, Johannesburg: Jonathan Ball, 2020.]
Commodity exports have been particularly hard hit, underlining the need for the diversification of Africa’s economies to reduce the ‘boom and bust’ cycle so evident across much of the continent's development pathway. Regional trade initiatives such as the African Continental Free Trade Area and technology offer particularly important avenues to boost manufacturing in Africa as firms overcome constraints imposed by narrow domestic markets. The crisis has, however, created new, cross-sectoral and multi-stakeholder platforms between business, governments,international partners and civil society. These offer important opportunities for new ways of managing the economy in the future.
Already the African Export-Import Bank (Afreximbank), UNECA and the AU are jointly advocating for the removal of trade tariffs and other restrictions on medical supplies in Africa in the context of the COVID-19 pandemic. [72The Presidency, South Africa: COVID-19: African Union Chair, President Ramaphosa, launches the Africa Medical Supplies Platform, Africa’s Unified Continental Response to fight the pandemic, 18 June 2020]
Similar to other regions, intra-African trade has relatively higher industrial content than Africa’s trade with the rest of the world. The result is that the opportunity to trade freely in a much larger region will increase the value-add of intra-African trade with each passing year. That, and the extent to which global value chains are shifting and manufacturing is shifting closer to the consumer, could all be to the continent’s advantage, but only if Africans make it clear that the continent is open for business.
African countries must push rapid digitisation as a pathway to more rapid and sustainable growth. Only a third of Africa is currently connected to the Internet and connections are often slow and unreliable. The Digital Transformation Strategy for Africa 2020 to 2030 already provides a framework for the development of a Digital Single Market for Africa and implementation must be speeded up. [73African Union, The Digital Transformation Strategy for Africa (2020-2030)]
African governments need to partner with the private sector to expand access through provision of more bandwidth and national access. Digitisation would unlock other productivity advancing initiatives such as in education and the more rapid formalisation of Africa’s large informal sector.
COVID-19 also underlines the need for a more rapid transition to renewable energy. For example, on 28 May 2020 the World Bank, International Energy Agency, World Health Organization and International Renewable Energy Agency issued a joint statement agreeing that the real lesson from COVID-19 is that investments in renewable energy, both for homes and business, have remained profitable, while those in fossil fuel projects have declined. [74The International Energy Agency, International Renewable Energy Agency, United Nations Statistics Division, World Bank and WHO, COVID-19 intensifies the urgency to expand sustainable energy solutions worldwide, 28 May 2020]
This study has sought to explore the potential impact of the COVID-19 pandemic on Africa, looking out to 2030 in terms of income, debt, poverty and some elements of the SDGs. The report is necessarily incomplete. It has, for example, not dealt with the food security crisis in the region that the World Bank estimates could follow a contraction in agricultural production of between 2.6% and 7% and reductions in food imports. It has also not fully unpacked the implications of large reductions in FDI as expected by the UN Conference on Trade and Development.
Nor has the report looked at the potential for social protection programmes to support workers, especially those in the informal sector. These could include measures such as cash transfers, in-kind transfers (food distribution), social grants to disabled people and the elderly, wage subsidies to prevent massive layoffs, and fee waivers for basic services.
The report finds that the pandemic is set to erase much of the progress made in the fight against poverty in recent years, setting back the attainment of the 2030 SDGs and Agenda 2063.
At the time of concluding the report, it is expected that the health situation will get significantly worse as infections and mortality rates from COVID-19 increase before they improve. However, it also offers the continent the opportunity to learn from the experience of others. Bad as it is, high mortality is not expected to be the main driver of suffering in Africa. That will largely come from the economic impact of COVID-19.
To avoid another lost decade, as in the 1980s, appropriate policies need to be implemented to mitigate the pandemic’s short-term negative socio-economic impact and to boost long-term growth. Policymakers should, therefore, strengthen national health systems and improve access to water and sanitation. Africa also needs to use digital technologies to accelerate its economic structural transformation. All of these should be underpinned by good governance and will require substantial debt relief.
This report sought to outline alternative prospects for Africa amid unprecedented levels of uncertainty, on a matter that changes on a daily basis. Some of our assumptions are certain to be proven incorrect and will need to be modified as our understanding of the unfolding pandemic improves.
Governments, civil society, and the business community need to forge a shared response to one of the greatest challenges humanity has faced in recent decades. It is our hope that by taking a long-term perspective rooted in available evidence, we might contribute to a sensible and effective response.
Annex 1
Extreme poverty under different scenarios (millions) using US$1.90
|
Country |
|
2019 |
2020 |
2025 |
2030 |
|
Algeria |
Pre-COVID |
0.012 |
0.014 |
0.017 |
0.010 |
|
V |
0.012 |
0.012 |
0.027 |
0.016 |
|
|
U |
0.012 |
0.012 |
0.034 |
0.019 |
|
|
L |
0.012 |
0.012 |
0.044 |
0.022 |
|
|
Angola |
Pre-COVID |
12.500 |
12.980 |
15.940 |
16.600 |
|
V |
12.500 |
13.190 |
16.250 |
17.090 |
|
|
U |
12.500 |
13.190 |
16.660 |
17.550 |
|
|
L |
12.500 |
13.190 |
16.940 |
17.890 |
|
|
Benin |
Pre-COVID |
5.717 |
5.860 |
6.441 |
7.037 |
|
V |
5.718 |
5.896 |
6.574 |
7.207 |
|
|
U |
5.718 |
5.896 |
6.594 |
7.231 |
|
|
L |
5.718 |
5.896 |
6.617 |
7.291 |
|
|
Botswana |
Pre-COVID |
0.267 |
0.261 |
0.211 |
0.177 |
|
V |
0.267 |
0.241 |
0.237 |
0.203 |
|
|
U |
0.267 |
0.241 |
0.270 |
0.228 |
|
|
L |
0.267 |
0.241 |
0.281 |
0.247 |
|
|
Burkina Faso |
Pre-COVID |
7.971 |
7.951 |
7.379 |
7.864 |
|
V |
7.971 |
8.051 |
7.674 |
8.281 |
|
|
U |
7.971 |
8.051 |
7.788 |
8.474 |
|
|
L |
7.971 |
8.051 |
7.885 |
8.662 |
|
|
Burundi |
Pre-COVID |
7.999 |
8.204 |
9.713 |
10.910 |
|
V |
8.000 |
8.529 |
9.939 |
11.040 |
|
|
U |
8.000 |
8.529 |
9.968 |
11.120 |
|
|
L |
8.000 |
8.529 |
10.010 |
11.200 |
|
|
Cameroon |
Pre-COVID |
5.914 |
6.002 |
6.315 |
6.596 |
|
V |
5.914 |
6.097 |
6.814 |
7.269 |
|
|
U |
5.914 |
6.097 |
7.051 |
7.615 |
|
|
L |
5.914 |
6.097 |
7.285 |
7.974 |
|
|
Cape Verde |
Pre-COVID |
0.038 |
0.039 |
0.031 |
0.031 |
|
V |
0.038 |
0.036 |
0.038 |
0.039 |
|
|
U |
0.038 |
0.036 |
0.039 |
0.044 |
|
|
L |
0.038 |
0.036 |
0.040 |
0.052 |
|
|
CAR |
Pre-COVID |
3.197 |
3.227 |
3.429 |
3.959 |
|
V |
3.197 |
3.264 |
3.511 |
4.085 |
|
|
U |
3.197 |
3.264 |
3.522 |
4.103 |
|
|
L |
3.197 |
3.264 |
3.544 |
4.137 |
|
|
Chad |
Pre-COVID |
6.568 |
6.892 |
7.649 |
9.024 |
|
V |
6.567 |
6.875 |
7.760 |
9.665 |
|
|
U |
6.567 |
6.875 |
8.053 |
9.840 |
|
|
L |
6.567 |
6.875 |
8.539 |
10.130 |
|
|
Comoros |
Pre-COVID |
0.167 |
0.170 |
0.198 |
0.213 |
|
V |
0.167 |
0.183 |
0.206 |
0.213 |
|
|
U |
0.167 |
0.183 |
0.210 |
0.218 |
|
|
L |
0.167 |
0.183 |
0.215 |
0.225 |
|
|
DR Congo |
Pre-COVID |
63.230 |
64.780 |
74.780 |
84.010 |
|
V |
63.250 |
65.490 |
77.360 |
88.850 |
|
|
U |
63.250 |
65.490 |
77.970 |
90.250 |
|
|
L |
63.250 |
65.490 |
78.570 |
92.300 |
|
|
Rep of Congo |
Pre-COVID |
2.018 |
2.055 |
2.433 |
2.839 |
|
V |
2.018 |
2.030 |
2.556 |
3.027 |
|
|
U |
2.018 |
2.030 |
2.634 |
3.115 |
|
|
L |
2.018 |
2.030 |
2.629 |
3.106 |
|
|
Côte d'Ivoire |
Pre-COVID |
5.665 |
5.739 |
4.855 |
4.321 |
|
V |
5.662 |
5.819 |
5.514 |
5.368 |
|
|
U |
5.662 |
5.819 |
6.012 |
5.858 |
|
|
L |
5.662 |
5.819 |
6.453 |
6.351 |
|
|
Djibouti |
Pre-COVID |
0.165 |
0.176 |
0.255 |
0.267 |
|
V |
0.165 |
0.189 |
0.265 |
0.287 |
|
|
U |
0.165 |
0.189 |
0.268 |
0.297 |
|
|
L |
0.165 |
0.189 |
0.270 |
0.307 |
|
|
Egypt |
Pre-COVID |
1.164 |
1.135 |
0.840 |
0.940 |
|
V |
1.164 |
1.188 |
1.103 |
1.255 |
|
|
U |
1.164 |
1.188 |
1.027 |
1.173 |
|
|
L |
1.164 |
1.188 |
1.110 |
1.249 |
|
|
Equatorial Guinea |
Pre-COVID |
0.000 |
0.000 |
0.000 |
0.000 |
|
V |
0.000 |
0.000 |
0.000 |
0.000 |
|
|
U |
0.000 |
0.000 |
0.000 |
0.000 |
|
|
L |
0.000 |
0.000 |
0.000 |
0.000 |
|
|
Eritrea |
Pre-COVID |
1.595 |
1.642 |
1.561 |
1.697 |
|
V |
1.597 |
1.674 |
1.599 |
1.791 |
|
|
U |
1.597 |
1.674 |
1.608 |
1.798 |
|
|
L |
1.597 |
1.674 |
1.743 |
1.902 |
|
|
Ethiopia |
Pre-COVID |
26.670 |
25.880 |
26.420 |
24.660 |
|
V |
26.670 |
25.740 |
27.870 |
26.430 |
|
|
U |
26.670 |
25.860 |
28.530 |
27.270 |
|
|
L |
26.670 |
25.740 |
29.060 |
28.160 |
|
|
Gabon |
Pre-COVID |
0.047 |
0.036 |
0.015 |
0.010 |
|
V |
0.047 |
0.029 |
0.017 |
0.012 |
|
|
U |
0.047 |
0.029 |
0.018 |
0.013 |
|
|
L |
0.047 |
0.029 |
0.019 |
0.014 |
|
|
Gambia |
Pre-COVID |
0.242 |
0.245 |
0.226 |
0.203 |
|
V |
0.242 |
0.260 |
0.243 |
0.230 |
|
|
U |
0.242 |
0.260 |
0.253 |
0.244 |
|
|
L |
0.242 |
0.260 |
0.262 |
0.257 |
|
|
Ghana |
Pre-COVID |
2.853 |
2.793 |
2.767 |
2.860 |
|
V |
2.852 |
2.704 |
3.007 |
3.101 |
|
|
U |
2.852 |
2.704 |
3.091 |
3.203 |
|
|
L |
2.852 |
2.704 |
3.161 |
3.290 |
|
|
Guinea |
Pre-COVID |
4.055 |
4.541 |
4.582 |
4.538 |
|
V |
4.055 |
4.659 |
4.854 |
4.845 |
|
|
U |
4.055 |
4.659 |
5.021 |
5.065 |
|
|
L |
4.055 |
4.659 |
4.822 |
5.123 |
|
|
Guinea-Bissau |
Pre-COVID |
1.227 |
1.228 |
1.236 |
1.300 |
|
V |
1.227 |
1.245 |
1.280 |
1.371 |
|
|
U |
1.227 |
1.245 |
1.299 |
1.401 |
|
|
L |
1.227 |
1.245 |
1.316 |
1.429 |
|
|
Kenya |
Pre-COVID |
18.010 |
18.200 |
17.830 |
18.400 |
|
V |
18.000 |
18.510 |
19.040 |
19.860 |
|
|
U |
18.000 |
18.510 |
19.560 |
20.570 |
|
|
L |
18.000 |
18.510 |
20.030 |
21.200 |
|
|
Lesotho |
Pre-COVID |
1.269 |
1.306 |
1.447 |
1.471 |
|
V |
1.269 |
1.319 |
1.430 |
1.500 |
|
|
U |
1.269 |
1.319 |
1.439 |
1.518 |
|
|
L |
1.269 |
1.319 |
1.456 |
1.557 |
|
|
Liberia |
Pre-COVID |
2.387 |
2.426 |
3.344 |
4.430 |
|
V |
2.386 |
2.543 |
3.318 |
4.519 |
|
|
U |
2.386 |
2.543 |
3.427 |
4.563 |
|
|
L |
2.386 |
2.543 |
3.422 |
4.544 |
|
|
Madagascar |
Pre-COVID |
19.990 |
20.380 |
22.230 |
25.600 |
|
V |
19.990 |
20.530 |
22.650 |
26.410 |
|
|
U |
19.990 |
20.530 |
22.910 |
26.840 |
|
|
L |
19.990 |
20.530 |
23.110 |
27.210 |
|
|
Malawi |
Pre-COVID |
12.400 |
12.390 |
13.250 |
13.760 |
|
V |
12.400 |
12.500 |
13.590 |
14.150 |
|
|
U |
12.400 |
12.500 |
13.440 |
14.110 |
|
|
L |
12.400 |
12.500 |
13.530 |
14.270 |
|
|
Mali |
Pre-COVID |
9.438 |
9.632 |
10.950 |
13.480 |
|
V |
9.437 |
9.795 |
11.330 |
14.010 |
|
|
U |
9.437 |
9.795 |
11.480 |
14.290 |
|
|
L |
9.437 |
9.795 |
11.590 |
14.550 |
|
|
Mauritania |
Pre-COVID |
0.271 |
0.285 |
0.435 |
0.323 |
|
V |
0.271 |
0.282 |
0.457 |
0.427 |
|
|
U |
0.271 |
0.282 |
0.495 |
0.467 |
|
|
L |
0.271 |
0.282 |
0.556 |
0.671 |
|
|
Mauritius |
Pre-COVID |
0.000 |
0.000 |
0.000 |
0.000 |
|
V |
0.000 |
0.001 |
0.000 |
0.000 |
|
|
U |
0.000 |
0.001 |
0.000 |
0.000 |
|
|
L |
0.000 |
0.001 |
0.000 |
0.000 |
|
|
Morocco |
Pre-COVID |
0.075 |
0.075 |
0.051 |
0.039 |
|
V |
0.075 |
0.055 |
0.067 |
0.049 |
|
|
U |
0.075 |
0.055 |
0.074 |
0.056 |
|
|
L |
0.075 |
0.055 |
0.079 |
0.063 |
|
|
Mozambique |
Pre-COVID |
18.890 |
19.460 |
22.230 |
25.180 |
|
V |
18.880 |
19.660 |
22.060 |
26.090 |
|
|
U |
18.880 |
19.660 |
22.170 |
26.290 |
|
|
L |
18.880 |
19.660 |
21.810 |
25.580 |
|
|
Namibia |
Pre-COVID |
0.402 |
0.444 |
0.537 |
0.537 |
|
V |
0.402 |
0.416 |
0.558 |
0.565 |
|
|
U |
0.402 |
0.416 |
0.569 |
0.580 |
|
|
L |
0.402 |
0.416 |
0.585 |
0.595 |
|
|
Niger |
Pre-COVID |
10.110 |
10.540 |
11.800 |
14.260 |
|
V |
10.110 |
10.860 |
13.280 |
17.510 |
|
|
U |
10.110 |
10.860 |
12.280 |
15.640 |
|
|
L |
10.110 |
10.860 |
13.720 |
18.620 |
|
|
Nigeria |
Pre-COVID |
107.900 |
110.500 |
125.800 |
137.600 |
|
V |
107.900 |
118.700 |
132.000 |
147.900 |
|
|
U |
107.900 |
118.700 |
135.200 |
152.600 |
|
|
L |
107.900 |
118.700 |
137.800 |
158.400 |
|
|
Rwanda |
Pre-COVID |
6.004 |
5.925 |
5.559 |
5.547 |
|
V |
6.003 |
5.949 |
5.819 |
5.910 |
|
|
U |
6.003 |
5.949 |
5.932 |
6.110 |
|
|
L |
6.003 |
5.949 |
6.037 |
6.325 |
|
|
São Tomé and Príncipe |
Pre-COVID |
0.069 |
0.071 |
0.083 |
0.092 |
|
V |
0.075 |
0.080 |
0.093 |
0.108 |
|
|
U |
0.069 |
0.070 |
0.086 |
0.089 |
|
|
L |
0.075 |
0.080 |
0.094 |
0.109 |
|
|
Senegal |
Pre-COVID |
5.406 |
5.480 |
4.741 |
4.086 |
|
V |
5.405 |
5.542 |
4.928 |
4.327 |
|
|
U |
5.405 |
5.542 |
5.015 |
4.423 |
|
|
L |
5.405 |
5.542 |
4.978 |
4.377 |
|
|
Seychelles |
Pre-COVID |
0.000 |
0.000 |
0.000 |
0.000 |
|
V |
0.000 |
0.000 |
0.000 |
0.000 |
|
|
U |
0.000 |
0.000 |
0.000 |
0.000 |
|
|
L |
0.000 |
0.000 |
0.000 |
0.000 |
|
|
Sierra Leone |
Pre-COVID |
3.901 |
3.979 |
4.725 |
5.893 |
|
V |
3.901 |
4.323 |
5.093 |
6.319 |
|
|
U |
3.901 |
4.323 |
5.199 |
6.585 |
|
|
L |
3.901 |
4.323 |
5.182 |
7.054 |
|
|
Somalia |
Pre-COVID |
8.563 |
8.672 |
9.325 |
10.470 |
|
V |
8.565 |
9.195 |
9.541 |
11.170 |
|
|
U |
8.565 |
9.195 |
9.671 |
11.170 |
|
|
L |
8.565 |
9.195 |
9.883 |
11.180 |
|
|
South Africa |
Pre-COVID |
11.400 |
11.570 |
11.750 |
11.580 |
|
V |
11.400 |
11.700 |
12.980 |
12.510 |
|
|
U |
11.400 |
11.700 |
14.210 |
13.690 |
|
|
L |
11.400 |
11.700 |
15.260 |
14.710 |
|
|
Sudan |
Pre-COVID |
5.697 |
6.066 |
7.002 |
7.264 |
|
V |
5.693 |
6.932 |
7.752 |
8.328 |
|
|
U |
5.693 |
6.932 |
8.089 |
8.817 |
|
|
L |
5.693 |
6.932 |
8.466 |
9.441 |
|
|
South Sudan |
Pre-COVID |
6.294 |
5.819 |
4.157 |
3.222 |
|
V |
6.300 |
6.571 |
5.166 |
4.044 |
|
|
U |
6.300 |
6.571 |
5.475 |
4.491 |
|
|
L |
6.300 |
6.571 |
5.765 |
4.997 |
|
|
Eswatini |
Pre-COVID |
0.547 |
0.535 |
0.587 |
0.686 |
|
V |
0.547 |
0.529 |
0.617 |
0.728 |
|
|
U |
0.547 |
0.529 |
0.630 |
0.701 |
|
|
L |
0.547 |
0.529 |
0.618 |
0.689 |
|
|
Tanzania |
Pre-COVID |
25.180 |
25.140 |
23.940 |
23.320 |
|
V |
25.180 |
25.190 |
25.000 |
24.680 |
|
|
U |
25.180 |
25.190 |
25.550 |
25.490 |
|
|
L |
25.180 |
25.190 |
25.980 |
26.290 |
|
|
Togo |
Pre-COVID |
4.033 |
4.186 |
4.733 |
5.198 |
|
V |
4.033 |
4.209 |
4.849 |
5.384 |
|
|
U |
4.033 |
4.209 |
4.887 |
5.493 |
|
|
L |
4.033 |
4.209 |
4.935 |
5.590 |
|
|
Tunisia |
Pre-COVID |
0.043 |
0.047 |
0.040 |
0.037 |
|
V |
0.043 |
0.049 |
0.052 |
0.051 |
|
|
U |
0.043 |
0.049 |
0.059 |
0.060 |
|
|
L |
0.043 |
0.049 |
0.070 |
0.071 |
|
|
Uganda |
Pre-COVID |
18.650 |
19.520 |
23.250 |
29.580 |
|
V |
18.650 |
19.360 |
24.040 |
30.510 |
|
|
U |
18.650 |
19.360 |
24.310 |
30.840 |
|
|
L |
18.650 |
19.360 |
24.200 |
30.720 |
|
|
Zambia |
Pre-COVID |
10.020 |
10.320 |
12.140 |
14.100 |
|
V |
10.020 |
10.260 |
12.610 |
14.580 |
|
|
U |
10.020 |
10.260 |
12.880 |
14.900 |
|
|
L |
10.020 |
10.260 |
12.960 |
15.080 |
|
|
Zimbabwe |
Pre-COVID |
2.872 |
3.077 |
3.359 |
3.393 |
|
V |
2.871 |
3.613 |
3.811 |
3.979 |
|
|
U |
2.871 |
3.613 |
3.988 |
4.273 |
|
|
L |
2.871 |
3.613 |
4.104 |
4.615 |
Annex B
Progress towards SDGs under different scenarios
|
Indicators |
Pre- COVID by 2030 |
V by 2030 |
U by 2030 |
L by 2030 |
Target Value |
|
Goal 1: POVERTY |
|
|
|
|
|
|
Indicator 1.1.1b - Percentage of population below $1.90 (2011$ PPP) per day; Lognormal |
33.5 |
35.39 |
36.13 |
37.15 |
3 |
|
Goal 2: HUNGER |
|
|
|
|
|
|
Indicator 2.1.1a - Percentage of undernourished population |
12.99 |
13.64 |
14.02 |
14.5 |
3 |
|
Indicator 2.2.2c - Severe Acute Malnutrition (weight for height <-3 SD) among children under 5 |
2.294 |
2.317 |
2.325 |
2.336 |
1 |
|
Goal 3: HEALTH |
|
|
|
|
|
|
Indicator 3.2.2 - Infant mortality rate in deaths per thousand newborns |
34.59 |
35.96 |
36.55 |
37.21 |
12 |
|
Indicator 3.3.1a - HIV cases as percentage of population |
1.461 |
1.461 |
1.461 |
1.461 |
0 |
|
Indicator 3.3.1b - AIDS death rate as percentage of population |
0.0319 |
0.0319 |
0.0319 |
0.0319 |
0 |
|
Indicator 3.3.3 - Malaria death rate per thousand |
0.3291 |
0.3487 |
0.3574 |
0.3682 |
0 |
|
Indicator 3.7.1 - Contraception use as percentage of fertile women |
41.52 |
40.62 |
40.23 |
39.79 |
97 |
|
Goal 4: EDUCATION |
|
|
|
|
|
|
Indicator 4.1.1c - Primary education gross completion rate - Total |
86.6 |
86.16 |
85.99 |
85.8 |
97 |
|
Indicator 4.1.1e - Lower secondary education graduation rate - Total |
53.95 |
53.04 |
52.65 |
52.23 |
97 |
|
Indicator 4.1.1g - Upper secondary education graduation rate - Total |
39.57 |
38.62 |
38.23 |
37.8 |
97 |
|
Indicator 4.5.1i - Upper secondary education gross enrolment rate parity index (female/male) |
0.9621 |
0.9597 |
0.9586 |
0.957 |
1 |
|
Indicator 4.5.1j - Upper secondary education graduation rate parity index (female/male) |
1.009 |
1.005 |
1.004 |
1.002 |
1 |
|
Indicator 4.5.1k - Years of education obtained by population 15+ parity index (female/male) |
0.8551 |
0.854 |
0.8536 |
0.8531 |
1 |
|
Goal 6: WATER AND SANITATION |
|
|
|
|
|
|
Indicator 6.1.1 - Percentage of people with access to improved water |
83.2 |
82.5 |
82.3 |
82.1 |
98 |
|
Indicator 6.2.1 - Percentage of people with access to sanitation services - Improved |
50.0 |
48.2 |
47.6 |
47.1 |
98 |
|
Indicator 6.3.1a - Percentage of people connected to wastewater collection system |
21.6 |
21.4 |
21.3 |
21.3 |
98 |
|
Indicator 6.3.1b - Percentage of people connected to wastewater treatment system |
18.58 |
18.24 |
18.12 |
18 |
98 |
|
Goal 7: ENERGY |
|
|
|
|
|
|
Indicator 7.1.1 - Percentage of population with access to electricity - Total |
57.4 |
56.2 |
55.8 |
55.2 |
98 |
|
Indicator 7.2.1 - Renewable energy as percentage of total final energy consumption |
10.7 |
10.8 |
10.9 |
11.0 |
|
|
Goal 8: GROWTH AND EMPLOYMENT |
|
|
|
|
|
|
Indicator 8.1.1 - Annual growth rate of real GDP per capita |
1.925 |
1.813 |
1.65 |
1.568 |
|
|
Indicator 8.3.1 - Percentage of informal employment (non-agricultural) |
56.6 |
57.0 |
57.1 |
57.3 |
|
|
Goal 9: INFRASTRUCTURE; INDUSTRIALIZATION AND INNOVATION |
|
|
|
|
|
|
Indicator 9.2.1a - Manufacturing value added as a % of GDP |
18.9 |
18.7 |
18.7 |
18.6 |
|
|
Indicator 9.5.1 - Research and development spending as % of GDP |
0.4 |
0.4 |
0.4 |
0.4 |
|
|
Indicator 9.c.1b - Connections per hundred people to mobile broadband technology |
101.9 |
101.1 |
100.7 |
100.4 |
|
|
Goal 10: INEQUALITY |
|
|
|
|
|
|
Indicator 10.4.1b - Labour share of GDP; comprising wages and social protection transfers as percentage of GDP |
80.45 |
80.45 |
80.45 |
80.45 |
81 |
|
Goal 16: PEACE AND JUSTICE |
|
|
|
|
|
|
Indicator 16.1.1a - Number of victims of intentional injuries per thousand |
0.161 |
0.1621 |
0.1626 |
0.1632 |
|
|
Indicator 16.1.1b - Years of life lost to intentional injuries per thousand |
8.006 |
8.073 |
8.103 |
8.138 |
|
|
Goal 17: GLOBAL PARTNERSHIP |
|
|
|
|
|
|
Indicator 17.1.1a - Total government revenue as % of GDP |
26.2 |
26.3 |
26.4 |
26.5 |
|
|
Indicator 17.1.1b - Household taxes as % of GDP |
12.7 |
12.7 |
12.8 |
12.8 |
|
|
Indicator 17.1.1c - Firm taxes as % of GDP |
2.6 |
2.6 |
2.6 |
2.6 |
|
|
Indicator 17.1.2 - Percentage of domestic budget funded by domestic taxes |
98.5 |
99.7 |
100.3 |
101.1 |
|
Annex C
Adjustments made within IFs
Growth rate adjustments
The 2020 and 2021 growth rates for the following countries were adjusted to the June 2020 update from the IMF Selected Economies Real GDP Growth
- Egypt 2.0 in 2020 and 2021
- Nigeria -5.4 in 2020 and 2.6 in 2021
- South Africa -8.0 in 2020 and 3.5 in 2021
All adjustments are to gdprext with GDP adjustment switch gdpadsw set to 0.
Adjustments made in V scenario for 2021 to moderate the aggressive upward bounce in growth rates in that year. The adjustments revert the 2021 forecast to the IMF October 2019 growth forecast within IFs:
- Algeria from 6.196 to 1.754
- Burundi from 4.205 to 0.50
- Chad from 6.10 to 4.815
- Côte d’Ivoire from 3.039 to 7.006
- Djibouti from 8.499 to 6.00
- Equatorial Guinea from 2.289 to -5.261
- Eritrea from 5.901 to 4.03
- Ethiopia from 4.32 to 7.126
- Gambia from 6.501 to 5.60
- Ghana from 5.90 to 4.222
- Guinea from 7.60 to 5.99
- Guinea-Bissau from 3.005 to 5
- Lesotho from 5.142 to 3.68
- Liberia from 4.063 to 1.253
- Malawi from 2.50 to 5.5
- Mauritania from 4.20 to 5.851
- Mauritius from 5.90 to 3.93
- Morocco from 4.8 to 4.13
- Mozambique from 4.70 to 4
- Namibia from 3.20 to 2.433
- Niger from 8.103 to 5.594 also in 2022 from 11.9 to 5.83 to correct growth spike
- Republic of Congo from 3.40 to 1.92
- Rwanda from 6.70 to 8.20
- São Tomé and Príncipe from 6.726 to 4.00 also in 2019 from 10.11 to 3.0855 to correct growth spike
- Senegal from 5.50 to 6.959
- Seychelles from 8.015 to 4.024
- South Sudan from -2.986 to 5.015
- Sudan from -3 to -1.065
- Eswatini from 4.929 to 0.638
- Tanzania from 4.60 to 5.99
- Togo from 4.001 to 5.41
- Tunisia from 4.1 to 2.889
- Uganda from 4.40 to 6.142
- Angola from 2.6 to 2.874
- Mali from 4.1 to 4.9
- Sierra Leone from 4.002 to 4.782
- Cameroon from 4.1 to 4.511
- Chad from 6.1 to 4.815
- Kenya from 6.1 to 5.815
- DR Congo from 3.5 to 3.393
In the U scenario IFs interpolates growth rates from 2020 to 2021.
Country growth rates for U and L scenarios
|
|
For U scenario |
For L scenario |
|||||
|
|
2020 |
2021 |
2022 |
2020 |
2021 |
2022 |
2023 |
|
Algeria |
-5.20 |
-1.90 |
1.40 |
-5.20 |
-3.13 |
-1.07 |
1.00 |
|
Angola |
-1.40 |
0.95 |
3.30 |
-1.40 |
0.43 |
2.27 |
4.10 |
|
Benin |
4.50 |
5.60 |
6.70 |
4.50 |
5.23 |
5.97 |
6.70 |
|
Botswana |
-5.40 |
-0.75 |
3.90 |
-5.40 |
-2.30 |
0.80 |
3.90 |
|
Burkina Faso |
2.00 |
4.00 |
6.00 |
2.00 |
3.33 |
4.67 |
6.00 |
|
Burundi |
-5.50 |
-2.50 |
0.50 |
-5.50 |
-3.50 |
-1.50 |
0.50 |
|
Cameroon |
-1.20 |
1.90 |
5.00 |
-1.20 |
0.93 |
3.07 |
5.20 |
|
Cape Verde |
-6.20 |
-0.60 |
5.00 |
-6.20 |
-2.47 |
1.27 |
5.00 |
|
CAR |
1.00 |
3.00 |
5.00 |
1.00 |
2.33 |
3.67 |
5.00 |
|
Chad |
-0.20 |
2.55 |
5.30 |
-0.20 |
1.23 |
2.67 |
4.10 |
|
Comoros |
-1.20 |
1.15 |
3.50 |
-1.20 |
0.37 |
1.93 |
3.50 |
|
DR Congo |
-2.20 |
1.15 |
4.50 |
-2.20 |
-0.03 |
2.13 |
4.30 |
|
Congo, Republic of |
-2.30 |
-1.15 |
0.00 |
-2.30 |
-1.10 |
0.10 |
1.30 |
|
Côte d’Ivoire |
-3.30 |
1.70 |
6.70 |
-3.30 |
-0.03 |
3.23 |
6.50 |
|
Djibouti |
1.00 |
3.50 |
6.00 |
1.00 |
2.67 |
4.33 |
6.00 |
|
Egypt |
2.00 |
4.00 |
6.00 |
2.00 |
3.33 |
4.67 |
6.00 |
|
Equatorial Guinea |
-5.50 |
-5.55 |
-5.60 |
-5.50 |
-4.73 |
-3.97 |
-3.20 |
|
Eritrea |
0.10 |
3.65 |
7.20 |
0.10 |
1.63 |
3.17 |
4.70 |
|
Ethiopia |
3.20 |
5.10 |
7.00 |
3.20 |
4.33 |
5.47 |
6.60 |
|
Gabon |
-1.20 |
1.65 |
4.50 |
-1.20 |
0.70 |
2.60 |
4.50 |
|
Gambia |
2.50 |
3.95 |
5.40 |
2.50 |
3.37 |
4.24 |
5.10 |
|
Ghana |
1.50 |
3.05 |
4.60 |
1.50 |
2.67 |
3.83 |
5.00 |
|
Guinea |
2.90 |
4.10 |
5.30 |
2.90 |
3.60 |
4.30 |
5.00 |
|
Guinea-Bissau |
-1.50 |
1.80 |
5.10 |
-1.50 |
0.73 |
2.97 |
5.20 |
|
Kenya |
1.00 |
3.40 |
5.80 |
1.00 |
2.60 |
4.20 |
5.80 |
|
Lesotho |
-5.20 |
-0.35 |
4.50 |
-5.20 |
-3.00 |
-0.80 |
1.40 |
|
Liberia |
-2.50 |
-1.90 |
-1.30 |
-2.50 |
-1.84 |
-1.17 |
-0.50 |
|
Madagascar |
0.40 |
2.65 |
4.90 |
0.40 |
1.87 |
3.33 |
4.80 |
|
Malawi |
1.00 |
3.50 |
6.00 |
1.00 |
2.83 |
4.67 |
6.50 |
|
Mali |
1.50 |
3.20 |
4.90 |
1.50 |
2.60 |
3.70 |
4.80 |
|
Mauritania |
-2.00 |
3.60 |
9.20 |
-2.00 |
0.83 |
3.67 |
6.50 |
|
Mauritius |
-6.80 |
-1.40 |
4.00 |
-6.80 |
-3.20 |
0.40 |
4.00 |
|
Morocco |
-3.70 |
0.30 |
4.30 |
-3.70 |
-1.00 |
1.70 |
4.40 |
|
Mozambique |
2.20 |
3.10 |
4.00 |
2.20 |
4.53 |
6.87 |
9.20 |
|
Namibia |
-2.50 |
0.35 |
3.20 |
-2.50 |
-0.37 |
1.77 |
3.90 |
|
Niger |
1.00 |
6.45 |
11.90 |
1.00 |
2.70 |
4.40 |
6.10 |
|
Nigeria |
-5.40 |
-1.35 |
2.70 |
-5.40 |
-2.73 |
-0.07 |
2.60 |
|
Rwanda |
3.50 |
5.75 |
8.00 |
3.50 |
4.83 |
6.17 |
7.50 |
|
São Tomé and Príncipe |
3.52 |
4.02 |
4.51 |
3.52 |
3.84 |
4.17 |
4.50 |
|
Senegal |
3.00 |
5.70 |
8.40 |
3.00 |
5.87 |
8.73 |
11.60 |
|
Seychelles |
-10.80 |
-3.40 |
4.00 |
-10.80 |
-5.93 |
-1.07 |
3.80 |
|
Sierra Leone |
-2.30 |
1.15 |
4.60 |
-2.30 |
0.03 |
2.37 |
4.70 |
|
Somalia |
-2.50 |
0.50 |
3.50 |
-2.50 |
-0.50 |
1.50 |
3.50 |
|
South Africa |
-8.00 |
-3.10 |
1.80 |
-8.00 |
-4.73 |
-1.47 |
1.80 |
|
Sudan |
-7.20 |
-3.50 |
0.20 |
-7.20 |
-4.47 |
-1.73 |
1.00 |
|
Sudan South |
-7.20 |
-0.65 |
5.90 |
-7.20 |
-3.03 |
1.13 |
5.30 |
|
Eswatini |
-4.90 |
-2.20 |
0.50 |
-4.90 |
-3.07 |
-1.23 |
0.60 |
|
Tanzania |
2.00 |
4.15 |
6.30 |
2.00 |
3.50 |
5.00 |
6.50 |
|
Togo |
1.00 |
3.20 |
5.40 |
1.00 |
2.47 |
3.93 |
5.40 |
|
Tunisia |
-4.30 |
-0.25 |
3.80 |
-4.30 |
-1.57 |
1.17 |
3.90 |
|
Uganda |
3.50 |
4.80 |
6.10 |
3.50 |
4.93 |
6.37 |
7.80 |
|
Zambia |
-3.50 |
-0.95 |
1.60 |
-3.50 |
-1.83 |
-0.17 |
1.50 |
|
Zimbabwe |
-7.40 |
-2.45 |
2.50 |
-7.40 |
-4.20 |
-1.00 |
2.20 |
Mortality
Respiratory infections (hlmortm) were adjusted as follows for Africa (without Libya):
- V: 1.375 in 2020
- U: 2.039 in 2020 and interpolate to 1 over two years
- L: 2.69 in 2020 and interpolate to 1 over three years
Additional social grants
The data for additional social grants is taken from IMF, Policy Responses to COVID-19, at www.imf.org/en/Topics/imf-and-covid19/Policy-Responses-to-COVID-19.
The 2020 values in IFs for govhhtrmwelm for countries where data is available are listed in the table below and used for all three scenarios. The value for all other countries was set at an average of 1.1794. In the U scenario the additional social grants were interpolated to 1 in 2022. In the L scenario the additional social grants were interpolated to 1 in 2023.
|
|
2020 value |
|
Algeria |
1.0112 |
|
Chad |
1.2 |
|
Egypt |
1.001 |
|
Ethiopia |
1.23 |
|
Kenya |
1.018 |
|
Malawi |
1.39 |
|
Mauritius |
1.85 |
|
Nigeria |
1.013 |
|
Senegal |
1.05 |
|
South Africa |
1.169 |
|
Sudan |
1.8 |
|
Tunisia |
1.045 |
Endnotes
For a useful mapping of the Sustainable Development Goals and targets to the African Union’s Agenda 2063, see: United Nations Economic Commission for Africa (UNECA), Integrating Agenda 2063 and 2030 Agenda for Sustainable Development into national development plans, 2017
Algeria, Tunisia, Mali, Sierra Leone, Nigeria, Cameroon, Chad, Sudan, Ethiopia, Kenya, the Democratic Republic of the Congo (DR Congo), Angola, Malawi, South Africa and Mauritius.
Africa Centres for Disease Control and Prevention (CDC), Coronavirus Disease 2019 (COVID-19)
WHO, Rolling updates on coronavirus disease (COVID-19)
United Nations, UN launches COVID-19 plan that could ‘defeat the virus and build a better world’, UN News, 31 March 2020
International Monetary Fund (IMF), Confronting the Crisis: Priorities for the Global Economy, speech by Kristalina Georgieva, IMF managing director, Washington, DC, 2020
United Nations Development Programme (UNDP), Human Development Reports, COVID-19 and Human Development: Assessing the Crisis, Envisioning the Recovery, 2020, p.6
Average health expenditure in sub-Saharan Africa is roughly 2.6% of GDP. It is three times that in North America and in Europe.
Africa Center for Strategic Studies, African Adaptations to the COVID-19 Response, 15 April
A Otu, B Ebenso, R Labonte and S Yaya, Tackling COVID-19: Can the African continent play the long game?, Journal of Global Health, 10:1, 2020, 10339. Note: Chikungunya is a viral disease transmitted to humans by infected mosquitoes. It has been identified in over 60 countries globally, including most prominently in the DR Congo and Gabon. Lassa fever is an acute viral haemorrhagic illness caused by the Lassa virus. It is endemic in Benin, Ghana, Guinea, Liberia, Mali, Sierra Leone, Togo and Nigeria.
World Health Organization (WHO), WHO welcomes preliminary results about dexamethasone use in treating critically ill COVID-19 patients, 16 June 2020
R Haussman, Managing COVID-19 in the Americas, Africa and the Middle East, 29 May 2020
Note that the IMF October 2019 forecast is out to 2024. The forecast beyond that is from IFs.
G Paravicini, All African countries now have coronavirus lab testing capacity - WHO chief, Reuters, 24 June 2020;
African countries move from COVID-19 readiness to response as many confirm cases, WHOWHO, African countries move from COVID-19 readiness to response as many confirm cases
For a summary of thinking in this regard see L Spinney, Are we underestimating how many people are resistant to Covid-19?, The Guardian, 7 June 2020
This includes 47 African countries with roughly one billion people, excluding Djibouti, Egypt, Libya, Morocco, Somalia, Sudan and Tunisia.
JW Cabore et al, The potential effects of widespread community transmission of SARS-CoV-2 infection in the World Health Organization African Region: A predictive model, BMJ Global Health, 2020.
K Alcorn, People with HIV at greater risk of COVID-19 death in South African study, NAMAidsmap, 10 June 2020
S Ghisolfi et al, Predicted COVID-19 Fatality Rates Based on Age, Sex, Comorbidities, and Health System Capacity, Center for Global Development, Working Paper 535, 12 June 2020, 2
J Sandefur et al, Predicting COVID-19 Infection Fatality Rates Around the World, Center for Global Development, 12 June 2020
According to the WHO: ‘The new estimates are based on modifying the risk of transmission and disease severity by variables specific to each country in order to adjust for the unique nature of the region. The model predicts the observed slower rate of transmission, lower age of people with severe disease and lower mortality rates compared to what is seen in the most affected countries in the rest of the world. This is largely driven by social and environmental factors slowing the transmission, and a younger population that has benefited from the control of communicable diseases such as HIV and tuberculosis to reduce possible vulnerabilities.’ Smaller African countries alongside Algeria, South Africa and Cameroon were at high risk if containment measures were not prioritised, the WHO noted. The WHO study looked at 47 countries in the WHO African Region with a total population of one billion whereas the other studies were on all of Africa. WHO, New WHO estimates: Up to 190 000 people could die of COVID-19 in Africa if not controlled, COVID-19, 7 May 2020
Modelling done by a consortium from three universities in South Africa considers a likely total 2020 mortality of between 34 015 and 49 774 in that country by November 2020. L López González, Read South Africa’s national, provincial COVID-19 projections in full, Bhekisisa Centre for Health Journalism, 20 May 2020. The additional respiratory infection for South Africa in our modelling for the V scenario is 16 610, in the U scenario it is 43 740 and in the L scenario it is 70 340 for 2020.
UNECA, COVID-19 in Africa: Protecting Lives and Economies in Africa, April 2020, 8. UNECA relied on the Imperial College infection and mortality results and modelled three scenarios at the continental level.
2014–2016 Ebola Outbreak in West Africa, Centers for Disease Control and Prevention, 8 March 2019
S Davies and B Bennett, A Gendered Human Rights Analysis of Ebola and Zika: Locating Gender in Global Health Emergencies, International Affairs, 92:5, 2016, 1041–60, reported in J Smith, Overcoming the ‘Tyranny of the Urgent’: Integrating Gender into Disease Outbreak Preparedness and Response, Gender & Development, 27:2.
Joint United Nations Programme on HIV/AIDS (UNAIDS), The cost of inaction: COVID-19-related service disruptions could cause hundreds of thousands of extra deaths from HIV, 11 May 2020
Total additional mortality for V over the period 2020 to 2030 is 1 834 700 deaths, of which 642 300 are from respiratory infections. The numbers for U are 3 280 800 and 1 757 200. The numbers for L are 5 278 300 and 3 428 500.
For an explanation and illustration of the associated methodology, see: US National Center for Health Statistics, Excess Deaths Associated with COVID-19, 2020
R Maclean, Covid-19 outbreak in Nigeria is just one of Africa’s alarming hot spots, New York Times, 17 May 2020. In 2017, during an evaluation of its capacity to prevent, detect and respond to public health risks, Nigeria had scored poorly in both prevention and response. See S Dixit, Y Ogundeji and O Onwujekwe, How well has Nigeria responded to COVID-19?, 2 July 2020
Tracking covid-19 excess deaths across countries, The Economist, 13 June 2020
Center for Global Development, UNECA executive secretary Vera Songwe in conversation with Masood Ahmed, 17 June 2020
The tax-to-GDP ratio in Africa is the lowest of any region globally at 13.4% in 2018, compared to 14% in Asia, 25% in Europe, and 18% in Latin America.
Center for Global Development, UNECA executive secretary Vera Songwe in conversation with Masood Ahmed, 17 June 2020; P Madden, Figures of the week: Africa’s fiscal response to COVID-19, 13 May 2020
For a summary of country-level responses see: IMF, Policy Responses to COVID
Equivalent to 0.05 percentage points.
J Moyer and S Hedden, Are we on the right path to achieve the sustainable development goals? World Development, Volume 127, March 2020
According to the World Bank: ‘The 2020 downturn will likely increase the SSA poverty rate by at least 2 percentage points. This would mean that an additional 26 million people in SSA would fall into extreme poverty (defined as those living under US$1.90 per day in 2011 PPP). This projected increase in the poverty rate would return SSA to 2015 poverty levels, effectively wiping out 5 years of progress reducing impoverishment.’ J Montes et al, Poverty & Equity Notes, World Bank Group, Number 20, May 2020, 3.
Africa’s population is currently at 1.343 billion and should increase to 1.710 billion by 2030.
To 233 million, 239 million or 247 million in the V-, U- and L scenarios respectively.
UN World Tourism Organization, International Tourism and COVID-19
According to the World Bank, global remittances would experience the sharpest decline in recent history, falling by one fifth in 2020. Its forecast for sub-Saharan Africa is a decline of 23.1% in 2020 and a decline of 19.6% in North Africa and the Middle East. The outlook for 2021 is uncertain, but the World Bank expects a recovery of 4% in sub-Saharan Africa and 1.6% in North Africa. World Bank Group, World Bank predicts sharpest decline of remittances in recent history, 22 April 2020.
Report on the coordination meeting of the African Union Development Agency (AUDA-NEPAD) with the AU Regional Economic Communities (RECs) under the patronage of the chairperson of the African Union Commission (AUC): The Regional Response to COVID-19 held on 18 May 2020, 3.
M Mutize, African countries aren’t borrowing too much: They’re paying too much for debt, The Conversation, 19 February 2020
C Onyekwena and MA Ekeruche, Is a debt crisis looming in Africa?, 10 April 2019
UN, Sudan: Coronavirus could be tipping point for ‘untold suffering’, Bachelet urges sanctions relief, UN News, 28 April 2020
J Mutua, SGR services at risk over Sh38bn China firm debt, 10 June 2020
K Georgieva, Opening Remarks at High-Level Virtual Event on ‘Mobilizing with Africa’, 17 April 2020
The World Bank, For Sub-Saharan Africa, Coronavirus Crisis Calls for Policies for Greater Resilience, April 2020
The World Bank, COVID-19: Debt Service Suspension Initiative, 29 June 2020
D Malpass, Debt and investment transparency for better outcomes, World Bank blogs, 19 June 2020
This is through the Debt Service Suspension Initiative, T Maeko, Manuel: African nations need $40bn for debt relief, Mail & Guardian, 19 June 2020
C van Staden, Not much give from China in its relationship with Africa, Daily Maverick, 28 June 2020
S Morris, C Landers and A Gardner, More World Bank borrowers will need grants, not loans. as a result, more world bank donors will need to pony up, Center for Global Development, 4 June 2020
The World Bank, Debt Service Suspension and COVID-19, May 2020
See, for example: WHO, The Abuja Declaration: Ten Years On, 2011. Within IFs the following countries have government expenditure in excess of 15%: Eswatini, Malawi, The Gambia, Algeria, Lesotho, Republic of Congo, Ethiopia, São Tomé and Príncipe, Kenya, South Africa, Cape Verde, Niger, Rwanda and Zambia; Y Adegoke, African economies are spending up to five times their health budgets on debt repayments, QuartzAfrica, 30 April 2020
For example, the Health Finance and Governance project that analysed 43 of sub-Saharan Africa’s health financing outlooks found that 13 had reached the internationally accepted target of US$60 per capita health spending. It projected that nine additional countries would reach this target by 2020 on the assumption that health expenditure would follow increases in economic growth. Health Finance and Governance, Universal Coverage of Essential Health Services in Sub-Saharan Africa: Projections of Domestic Resources, United States Agency for International Development (USAID), 2013
Between 1.5% and 3% of GDP additional health financing is required to adequately respond to COVID-19 over a period of 250 days. In a Suppression scenario where wide-scale aggressive social distancing is pursued, an additional roughly US$23.54 billion would be required to prepare and treat the disease, and in a Social distancing scenario US$53 billion would be the target. P Schneider, F Pivodic and K Jison Yoo, How much health financing does Sub-Saharan Africa need to fight COVID-19 (coronavirus)?, World Bank Blogs, 15 April 2020
AB Hogan et al, The Potential Impact of the COVID-19 Epidemic on HIV, TB and Malaria in Low- and Middle-Income Countries, Report 19, Imperial College London, 1 May 2020
AB Hogan et al, The Potential Impact of the COVID-19 Epidemic on HIV, TB and Malaria in Low- and Middle-Income Countries, Report 19, Imperial College London, 1 May 2020
UNDP, Human Development Reports, COVID-19 and Human Development: Assessing the Crisis, Envisioning the Recovery, 2020, 12
WHO, Draft landscape of COVID-19 candidate vaccines, 24 June 2020
United Nations Conference on Trade and Development, COVID-19 heightens need for pharmaceutical production in poor countries, 27 May 2020
UNCTAC, COVID-19 heightens need for pharmaceutical production in poor countries, 27 May 2020. Also Gavi, Gavi launches innovative financing mechanism for access to COVID-19 vaccines
Africa is home to 90% or 380 000 of all malaria deaths in 2018. See: E Sherrard-Smith et al, The Potential Public Health Impact of COVID-19 on Malaria in Africa, Report 18, Imperial College London, 1 May 2020
TJ Bollyky, Plagues and the Paradox of Progress Why the World Is Getting Healthier in Worrisome Ways, Cambridge: MIT Press, 2018.
UN Department of Economic and Social Affairs, Population Division, 2018
J Stoler, WE Jepson and A Wutich, Beyond Handwashing: Water Insecurity Undermines COVID-19 Response in Developing Areas, Journal of Global Health, 15 May 2020
F Ndaw, COVID-19: Solving Africa’s water crisis is more urgent than ever, April 2020
See, for example: GSMA, Digital Solutions for the Urban Poor, 10 March 2020
J Cilliers, Africa First! Igniting a Growth Revolution, Johannesburg: Jonathan Ball, 2020.
The Presidency, South Africa: COVID-19: African Union Chair, President Ramaphosa, launches the Africa Medical Supplies Platform, Africa’s Unified Continental Response to fight the pandemic, 18 June 2020
African Union, The Digital Transformation Strategy for Africa (2020-2030)
The International Energy Agency, International Renewable Energy Agency, United Nations Statistics Division, World Bank and WHO, COVID-19 intensifies the urgency to expand sustainable energy solutions worldwide, 28 May 2020
Page information
Contact at AFI team is Jakkie Cilliers
This entry was last updated on 15 May 2023 using IFs v7.45.
Reuse our work
- All visualizations, data, and text produced by African Futures are completely open access under the Creative Commons BY license. You have the permission to use, distribute, and reproduce these in any medium, provided the source and authors are credited.
- The data produced by third parties and made available by African Futures is subject to the license terms from the original third-party authors. We will always indicate the original source of the data in our documentation, so you should always check the license of any such third-party data before use and redistribution.
- All of our charts can be embedded in any site.
Cite this research
Jakkie Cilliers (2024) Impact of COVID-19 in Africa: A scenario analysis to 2030 (July 2020). Published online at futures.issafrica.org. Retrieved from https://futures.issafrica.org/special-reports/other/covid/ [Online Resource] Updated 15 May 2023.